Abstract
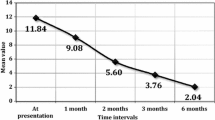
The aim of this study was to evaluate the effect of laparoscopic antireflux surgery (LARS) on the laryngeal symptoms, physical findings and voice parameters of gastroesophageal reflux disease (GERD) patients with or without laryngopharyngeal reflux (LPR). Forty-one GERD patients predominantly with LPR symptoms (Group I) and twenty-six GERD patients without LPR symptoms (Group II) who had LARS were prospectively analysed before and 2 years after the surgery. Upper gastrointestinal endoscopy, 24-h ambulatory pH or MII-pH monitoring was performed in all cases. A reflux study group including specialists from five departments in a university hospital decided surgical indications. Patients were asked to fill out a validated LPR and voice quality questionnaire (Reflux Symptom Index and Voice Handicap Index-10). Laryngeal findings were evaluated and scored using a laryngoscopic grading scale [Reflux Finding Score (RFS)], by four blinded ENT specialists. GRBAS scale was done by a blinded otolaryngologist. Voice parameters were measured objectively via the Multi Dimensional Voice Programme (MDVP). The mean age was 45.8 ± 8.5 for Group I (24 men) and 48.9 ± 12.3 for Group II (16 men). The mean follow-up after LARS was 24.5 ± 1.3 months for Group I and 25.2 ± 1.1 months for Group II. The preoperative mean score of RSI was 22.8 ± 7.4 vs. 11.2 ± 6.6; RFS was 10.6 ± 2.3 vs. 5.7 ± 2.5 and VHI was 18.07 ± 4.4 vs. 10.86 ± 3.3 for Group I and II, respectively. The postoperative mean score of RSI was 12.9 ± 6.4 vs. 8.4 ± 4.5; RFS was 6.9 ± 2.0 vs. 4.5 ± 2.3 and VHI was 9.59 ± 4.4 vs. 7.95 ± 3.5 for Group I and II, respectively. Group I had significantly lower RSI and RFS scores following LARS compared to the preoperative scores. LARS successfully improved RFS, RSI and VHI in carefully selected patients with GERD, especially the signs and symptoms related to the larynx and voice. Although the indications for LARS are limited in patients with LPR symptoms, these results favor the decision-making period of LARS.
Similar content being viewed by others
References
Bor S, Mandiracioglu A, Kitapcioglu G, Caymaz-Bor C, Gilbert RJ (2005) Gastresophageal reflux disease in a low-income region in Turkey. Am J Gastroenterol 100(4):759–765
Altman K, Prufer N, Vaezi M (2011) A review of clinical practice guidelines for reflux disease: toward creating a clinical protocol for the otolaryngologist. Laryngoscope 121:717–723
Vaezi MF, Hicks DM, Abelson TI, Richter JE (2003) Laryngeal signs and symptoms and gastroesophageal reflux disease (GERD). A critical assessment of cause and effect association. Clin Gastroenterol Hepatol 1:333–344
Poelmans J, Feenstra L, Tack J (2006) Determinants of long-term outcome of patients with reflux-related ear, nose, and throat symptoms. Dig Dis Sci 51(2):282–288
DeVault KR (2000) Overview of therapy for the extraesophageal manifestations of gastroesophageal reflux disease. Am J Gastrol 95:39–44
Maronian NC, Azadeh H, Waugh P, Hillel A (2001) Association of laryngopharyngeal reflux disease and subglottic stenosis. Ann Otol Rhinol Laryngol 110:606–612
Lewin JS et al (2003) Characterization of laryngopharyngeal reflux in patients with premalignant or early carcinomas of the larynx. Cancer 97(4):1010–1014
Barry DW, Vaezi MF (2010) Laryngopharyngeal reflux: more question than answers. Cleve Clin J Med 77:327–334
Carroll TL, Fedore LW, Aldahlawi MM (2012) pH Impedance and high-resolution manometry in laryngopharyngeal reflux disease high-dose proton pump inhibitor failures. Laryngoscope 122(11):2473–2481
Bilgen C, Ogut F, Kesimli-Dinc H, Kirazli T, Bor S (2003) The comparison of an empiric proton pump inhibitor trial vs. 24-h double-probe Ph monitoring in laryngopharyngeal reflux. J Laryngol Otol 117(5):386–390
Liakakos T, Karamanolis G, Patapis P, Misiakos EP (2009) Gastroesophageal reflux disease: medical or surgical treatment? Gastroenterol Res Pract. doi:10.1155/2009/371580
Ruiz-Tovar J, Diez-Tabernilla M, Chames A, Morales V, Martinez-Molina E (2010) Clinical outcome at 10 years after laparoscopic versus open Nissen fundoplication. J Laparoendosc Adv Surg Tech A 20(1):21–23
Belafsky PC, Postma GN, Koufman JA (2001) The validity and reliability of the Reflux Finding Score (RFS). Laryngoscope 111(8):1313–1317
Belafsky PC, Postma GN, Koufman JA (2002) Validity and reliability of the Reflux Symptom Index (RSI). J Voice 16:274–277
Kiliç MA, Okur E, Yildirim I, Oğüt F, Denizoğlu I, Kizilay A, Oğuz H, Kandoğan T, Doğan M, Akdoğan O, Bekiroğlu N, Oztarakçi H (2008) Reliability and validity of the Turkish version of the Voice Handicap Index. Kulak Burun Bogaz Ihtis Derg 18(3):139–147
Eadie T, Sroka A, Wright DR, Merati A (2011) Does knowledge of medical diagnosis bias auditory-percetual judgements of dysphonic voice. J Voice 25:420–429
Hicks DM, Ours TM, Abelson TI, Vaezi MF, Richter JE (2002) The prevelance of hypopharynx findings associated with reflux in normal volunteers. J Voice 16(4):564–579
Tamhankar AP, Peters JH, Portale G, Hsieh CC, Hagen JA, Bremner CG, DeMeester TR (2004) Omeprazole does not reduce gastroesophageal reflux: new insights using multichannel intraluminal impedance technology. J Gastrointest Surg 8:890–897
Sasaki CT, Marotta J, Hundal J, Chow J, Eisen RN (2005) Bile-induced laryngitis: is there a basis in evidence? Ann Otol Rhinol Laryngol 114:192–197
Amin MR, Postma GN, Johnson P, Digges N, Koufman JA (2001) Proton pump inhibitor resistance in the treatment of laryngopharyngeal reflux. Otolaryngol Head Neck Surg 125(4):374–378
Carlson MA, Frantzides CT (2001) Complications and results of primary minimally invasive anti-reflux procedures: a review of 10. 735 reported cases. J Am Coll Surg 193:428–439
Chen RY, Thomas RJS (2000) Results of laparoscopic fundoplication where atypical symptoms coexist with oesophageal reflux. Aust N Z J Surg 70:840–842
Oelschlager BK, Eubanks TR, Oleynikov D, Pope C, Pellegrini CA (2002) Symptomatic and physiological outcomes after operative treatment for extraesophageal reflux. Surg Endosc 16(7):1032–1036
So JB, Zeitels SM, Rattner DW (1998) Outcomes of atypical sypmtoms attributed to gastroesophageal reflux treated by laparoscopic Nissen fundoplication. Surgery 124:28–32
Farrel TM, Richardson WS, Trus TL, Smith CD, Hunter JG (2001) Response of atypical symptoms of gastro-oesophageal reflux to antireflux surgery. Br J Surg 88(12):1649–1652
Westcott CJ, Hopkins MB, Bach K, Postma GN, Belafsky PC, Koufman JA (2004) Fundoplication for laryngopharyngeal reflux disease. J Am Coll Surg 199(1):23–30
Qadeer MA et al (2005) Correlation between symptoms and laryngeal signs in laryngopharyngeal reflux. Laryngoscope 115(11):1947–1952
Catania RA et al (2007) Laparoscopic Nissen fundoplication effectively relieves symptoms in patients with laryngopharyngeal reflux. J Gastrointest Surg 11:1579–1588
Koufman JA, Amin MR, Panetti M (2000) Prevalence of reflux in 113 consecutive patients with laryngeal and voice disorders. Otolaryngol Head Neck Surg 123(4):385–388
Wiener GJ, Koufman JA, Wu WC et al (1989) Chronic hoarseness secondary to gastroesophageal reflux disease: documentation with 24-h ambulatory pH monitoring. Am J Gastroenterol 84:1503–1508
Ogut F, Ersin S, Engin EZ, Kirazli T, Midilli R, Unsal G, Bor S (2007) The effect of laparoscopic Nissen fundoplication on laryngeal findings and voice quality. Surg Endosc 21(4):549–554
Moon KR, Chung SM, Park HS, Kim HS (2012) Materials of acoustic analysis: sustained vowel versus sentence. J Voice 26(5):563–565
Arffa RE, Krishna P, Gardner-Schmidt J, Rosen CA (2012) Normative values for the Voice Handicap Index-10. J Voice 26(4):462–465
Granderath FA, Kamolz T, Schweiger UM, Pasiut M, Haas CF, Whkypiel H et al (2002) Long-term results of laparoscopic antireflux surgery. Surg Endosc 16:753–757
Singhal T, Balakrishnan S, Hussain A, Grandy-Smith S, Paix A, El-Hasani S (2009) Management of complications after laparoscopic Nissen’s fundoplication: a surgeon’s perspective. Ann Surg Innov Res 3:1. doi:10.1186/1750-1164-3-1
Conflict of interest
All authors have contributed significantly and all authors are in agreement with the content of the manuscript. This study does not have any financial support or relationships that may pose potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sahin, M., Vardar, R., Ersin, S. et al. The effect of antireflux surgery on laryngeal symptoms, findings and voice parameters. Eur Arch Otorhinolaryngol 272, 3375–3383 (2015). https://doi.org/10.1007/s00405-015-3657-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-015-3657-y