Abstract
Purpose
Umbilical hernias are common in young children. Many resolve spontaneously by age four with very low risk of symptoms or incarceration. Complications associated with surgical repair of asymptomatic umbilical hernias have not been well elucidated. We analyzed data from one hospital to test the hypothesis that repair at younger ages is associated with increased complication rates.
Methods
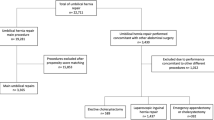
A retrospective chart review of all umbilical hernia repairs performed during 2007–2015 was conducted at a tertiary care children’s hospital. Patients undergoing repairs as a single procedure for asymptomatic hernia were evaluated for post-operative complications by age, demographics, and co-morbidities.
Results
Of 308 umbilical hernia repairs performed, 204 were isolated and asymptomatic. Postoperative complications were more frequent in children < 4 years (12.3%) compared to > 4 years (3.1%, p = 0.034). All respiratory complications (N = 4) and readmissions (N = 1) were in children < 4 years.
Conclusions
Age of umbilical hernia repair in children varied widely even within a single institution, demonstrating that timing of repair may be a surgeon-dependent decision. Patients < 4 years were more likely to experience post-operative complications. Umbilical hernias often resolve over time and can safely be monitored with watchful waiting. Formal guidelines are needed to support delayed repair and prevent unnecessary, potentially harmful operations.

Similar content being viewed by others
Abbreviations
- ICD-9:
-
International classification of diseases, ninth revision
- CPT:
-
Current procedural terminology
- FDA:
-
Food and Drug Administration
- ASA:
-
American Society of Anesthesiologists
References
Arias E (2015) United States life tables. Natl Vital Stat Rep 64:63
Keshtgar AS, Griffiths M (2003) Incarceration of umbilical hernia in children: is the trend increasing? Eur J Pediatr Surg Off J Aust Assoc Pediatr Surg Al Z Kinderchir 13:40–43
Mack NK (1945) The incidence of umbilical herniae in Africans. East Afr Med J 22:369–371
Zens T, Cartmill R, Nichol P, Kohler J (2017) Management of asymptomatic pediatric umbilical hernias: a systematic review. J Pediatr Surg 52:1723–1731
Sibley WL, Lynn HB, Harris LE (1964) A 25 year study of infantile umbilical hernia. Surgery 55:462–468
Morgan WW, White JJ, Stumbaugh S, Haller JA (1970) Prophylactic umbilical hernia repair in childhood to prevent adult incarceration. Surg Clin North Am 50:839–845
Lassaletta L, Fonkalsrud EW, Tovar JA et al (1975) The management of umbilicial hernias in infancy and childhood. J Pediatr Surg 10:405–409
Blumberg NA (1980) Infantile umbilical hernia. Surg Gynecol Obstet 150:187–192
Meier DE, OlaOlorun DA, Omodele RA et al (2001) Incidence of umbilical hernia in African children: redefinition of “normal” and reevaluation of indications for repair. World J Surg 25:645–648
Brown RA, Numanoglu A, Rode H (2006) Complicated umbilical hernia in childhood. South Afr J Surg Suid-Afr Tydskr Vir Chir 44:136–137
Zendejas B, Kuchena A, Onkendi EO et al (2011) Fifty-three-year experience with pediatric umbilical hernia repairs. J Pediatr Surg 46:2151–2156
Walker SH (1967) The natural history of umbilical hernia. A six-year follow up of 314 Negro children with this defect. Clin Pediatr (Phila) 6:29–32
HCUPnet Healthcare Cost and Utilization Project. In: HCUPnet. https://hcupnet.ahrq.gov. Accessed 13 Jun 2018
Vrsansky P, Bourdelat D (1997) Incarcerated umbilical hernia in children. Pediatr Surg Int 12:61–62
Chemaly M, El-Rajab MA, Ziade FM, Naja ZM (2014) Effect of one anesthetic exposure on long-term behavioral changes in children. J Clin Anesth 26:551–556
Flick RP, Katusic SK, Colligan RC et al (2011) Cognitive and behavioral outcomes after early exposure to anesthesia and surgery. Pediatrics 128:e1053–e1061
Wang X, Xu Z, Miao C-H (2014) Current clinical evidence on the effect of general anesthesia on neurodevelopment in children: an updated systematic review with meta-regression. PloS One 9:e85760
Zhang H, Du L, Du Z et al (2015) Association between childhood exposure to single general anesthesia and neurodevelopment: a systematic review and meta-analysis of cohort study. J Anesth 29:749–757
Mamie C, Habre W, Delhumeau C et al (2004) Incidence and risk factors of perioperative respiratory adverse events in children undergoing elective surgery. Paediatr Anaesth 14:218–224
Ezomike UO, Ituen MA, Ekpemo SC et al (2012) Profile of paediatric umbilical hernias managed at federal medical centre umuahia. Niger J Med J Natl Assoc Resid Dr Niger 21:350–352
Chirdan LB, Uba AF, Kidmas AT (2006) Incarcerated umbilical hernia in children. Eur J Pediatr Surg Off J Aust Assoc Pediatr Surg Al Z Kinderchir 16:45–48. https://doi.org/10.1055/s-2006-923792
Mawera G, Muguti GI (1994) Umbilical hernia in Bulawayo: some observations from a hospital based study. Cent Afr J Med 40:319–323
Ireland A, Gollow I, Gera P (2014) Low risk, but not no risk, of umbilical hernia complications requiring acute surgery in childhood. J Paediatr Child Health 50:291–293
Rappaport BA, Suresh S, Hertz S et al (2015) Anesthetic—clinical implications of animal models. N Engl J Med 372:796–797
Center for Drug Evaluation and Research Drug Safety and Availability - FDA Drug Safety Communication: FDA review results in new warnings about using general anesthetics and sedation drugs in young children and pregnant women. https://www.fda.gov/Drugs/DrugSafety/ucm532356.htm?source=govdelivery&utm_medium=email&utm_source=govdelivery. Accessed 18 May 2018
Ing C, DiMaggio C, Whitehouse A et al (2012) Long-term differences in language and cognitive function after childhood exposure to anesthesia. Pediatrics 130:e476–e485
Ing CH, DiMaggio CJ, Malacova E et al (2014) Comparative analysis of outcome measures used in examining neurodevelopmental effects of early childhood anesthesia exposure. Anesthesiology 120:1319–1332
McGowan FX, Davis PJ (2008) Anesthetic-related neurotoxicity in the developing infant: of mice, rats, monkeys and, possibly, humans. Anesth Analg 106:1599–1602
Stratmann G (2011) Review article: neurotoxicity of anesthetic drugs in the developing brain. Anesth Analg 113:1170–1179
Glatz P, Sandin RH, Pedersen NL et al (2017) Association of anesthesia and surgery during childhood with long-term academic performance. JAMA Pediatr 171:e163470
Ing C, Wall MM, DiMaggio CJ et al (2017) Latent class analysis of neuro developmental deficit after exposure to anesthesia in early childhood. J Neurosurg Anesthesiol 29:264–273
Sun LS, Li G, Miller TLK et al (2016) Association between a single general anesthesia exposure before age 36 months and neurocognitive outcomes in later childhood. JAMA 315:2312–2320
de Graaff JC, Pasma W, van Buuren S et al (2016) Reference values for noninvasive blood pressure in children during anesthesia: a multicentered retrospective observational cohort study. Anesthesiology 125:904–913
McCann ME, Schouten ANJ, Dobija N et al (2014) Infantile postoperative encephalopathy: perioperative factors as a cause for concern. Pediatrics 133:e751–e757
Vavilala MS, Lee LA, Lam AM (2003) The lower limit of cerebral autoregulation in children during sevoflurane anesthesia. J Neurosurg Anesthesiol 15:307–312
Rhondali O, Juhel S, Mathews S et al (2014) Impact of sevoflurane anesthesia on brain oxygenation in children younger than 2 years. Paediatr Anaesth 24:734–740
Hall DE, Roberts KB, Charney E (1981) Umbilical hernia: what happens after age 5 years? J Pediatr 98:415–417
Al-alami AA, Zestos MM, Baraka AS (2009) Pediatric laryngospasm: prevention and treatment. Curr Opin Anaesthesiol 22:388–395
Brown EG, Anderson JE, Burgess D et al (2017) Pediatric surgical readmissions: are they truly preventable? J Pediatr Surg 52:161–165
Acknowledgements
We thank Sara Fernandes-Taylor, PhD, for critical review of the manuscript.
Funding
This research did not receive any grant funding from agencies in the public, commercial, or not-for-profit sectors. It was supported in part by an unrestricted grant from the Cars Curing Kids Foundation.
Author information
Authors and Affiliations
Contributions
JEK, principal investigator, was involved in all aspects of conception and design, data analysis and interpretation, manuscript drafting and revisions, and final manuscript approval. TZ, primary contributor to this project, was involved in all aspects of conception and design, data acquisition, data analysis and interpretation, manuscript drafting and revisions, and final manuscript approval. AR contributed to experimental design, performed a significant component of primary chart review data collection, was integral to data analysis and manuscript writing/revisions, and gave final approval of the manuscript. RC contributed to data analysis, manuscript drafting and revisions, and gave final approval of the manuscript. DO, BM, PN assisted in conception and experimental design, data analysis and interpretation, manuscript drafting and revisions, and gave final approval of the manuscript, providing specific suggestions pertinent to their areas of specialty.
Corresponding author
Ethics declarations
Financial disclosure
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Conflict of interest
We have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Zens, T.J., Rogers, A., Cartmill, R. et al. Age-dependent outcomes in asymptomatic umbilical hernia repair. Pediatr Surg Int 35, 463–468 (2019). https://doi.org/10.1007/s00383-018-4413-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-018-4413-3