Abstract
Objective
To describe the pathophysiologic response in cerebral blood flow (CBF) and autoregulation after severe traumatic brain injury (TBI), Glasgow Coma Score (GCS) ≤8 on admission, in children, defining a baseline for future studies.
Methods
Retrospective chart review of 95 patients following TBI, ages 0.1–18.4 years (<5 years (n = 44), <2 years (n = 17)) for CBF using Xenon Computerized Tomography (XeCT) over a 10-year period and 6-month Glasgow Outcome Scores (GOS). A total of 140 CBF studies were performed variably from admission up to post injury day (PID) 9; 27 patients underwent repeat CBF study after PaCO2 was manipulated to determine CO2 vasoreactivity (CO2VR).
Results
Mean CBF on admission (PID 0, n = 26) was 32.05 ± 21.45 ml/100 g/min (mean ± SEM) and was ≤20 ml/100 g/min in eight patients. At PID 1–2, mean CBF increased to 55.36 ± 23.11 ml/100 g/min. There was significant differences in mean CBF of “favorable” outcomes (GOS ≥ 4) versus “unfavorable” outcome (GOS ≤ 3) (61.74 ± 18.27 vs. 46.54 ± 26.26, respectively (P = 0.01)). “Unfavorable” outcomes were seen in all patients with CBF ≤20 ml/100 mg/min during PID 0–2 and in 76.5% of children <2 years. CO2VR <2%/Torr PaCO2 within PID 0–2 was significantly associated with “unfavorable” outcome (P = 0.029).
Conclusion
Younger age, early or later low CBF, and CO2VR <2%/Torr PaCO2 were correlated with poorer outcomes in children. This represents the largest experience with XeCT CBF in children and confirms our preliminary report of low early CBF after TBI in children, disturbed CO2VR, and relationship of low CBF and unfavorable outcome.
Similar content being viewed by others
Introduction
Despite increased public prevention programs, medical and surgical advancements resulting in improved outcomes, traumatic brain injury (TBI) still remains a major cause of death and disability in young children [17]. Previous studies have shown that children tend to have better outcomes than adults after TBI [23]. However, previous work showed that the very young (<2 years of age) have a significantly poorer outcome when compared with older children [1]. Several other studies have found that these younger children are more susceptible to long-term deficits, with worse outcomes in terms of cognition, memory, and motor function [15, 22]. It is not clear whether this difference is due to the mechanism of injury or physiologic differences of the brain at different stages development. Unfortunately, while the only treatment for the primary neural injury in both adults and children is the prevention of the injury, the goal(s) of present-day clinical management is to improve outcome by minimizing the second insults and the impact of secondary injury on injured but viable tissue. It is imperative to expand our understanding of the mechanisms involved with this pathophysiologic response in children following TBI if we are to develop novel therapeutic interventions directed at lessening the effects of this secondary injury cascade to improve outcome.
Secondary neural injury/damage can be caused by a variety of factors; one such factor believed to be primarily involved is the effect of injury on cerebral blood flow (CBF) resulting in either excess perfusion (hyperemia) or inadequate perfusion (ischemia). While there have been a number of important papers that have examined the changes in CBF in children post-TBI [11, 27, 33], few measured CBF specifically but rather inferred CBF through indirect measures including cerebral perfusion pressure, blood flow velocity, and autoregulatory indices [21]. Even when CBF is quantified, most available techniques do not provide anatomic maps of CBF and this is an important limitation given the heterogeneity of damage in various brain regions. Additionally, it has been shown that poor cerebral autoregulation is associated with unfavorable outcomes in children [34–36]. Lastly, few of these studies evaluated children <2 years of age. We previously produced CBF maps using Xenon Computerized Tomography (XeCT) reported on a preliminary study [1] in young children (<8 years of age) that suggest provocative findings, such as low rather than high CBF. However a study with a larger subset of patients, across a greater age range was needed. In the present study, we sought to expand on our previous report with the goals to: (1) define changes in CBF and cerebral vasoreactivity over time in the different age subgroups following TBI, (2) correlate the relationships of these values with outcomes in these children, and (3) determine the potential benefit of XeCT as an imaging modality of CBF in children after severe TBI.
Materials and methods
Study population
We retrospectively analyzed data from the charts of all children referred and admitted to the Children’s Hospital of Pittsburgh from 1988 to 1998 with the diagnoses of severe TBI (GCS ≤8 at the time of admission) who had undergone serial CBF studies using the XeCT method. A total of 95 children of all ages who have suffered TBI and had XeCT CBF studies were included. Forty four children were <5 years of age with 17 of those children <2 years of age. Twenty-seven patients of the total cohort had studies to determine CO2VR with CBF assessments in response to PaCO2 changes. The children were stratified into two groups by age: <5 years old (Group I, n = 44); and ≥5 years old (Group II, n = 51) based on previous work showing that children ≤4 years old had poorer outcomes [22] and for later comparison to an ongoing clinical trial in children. The clinical record, including emergency room, intensive care unit, acute care facility, and outpatient records, was reviewed for the history, hospital course, physiologic variables at the time of the CBF study, and outcome. Following admission to the emergency department, the severity of the injury was scored for all of the children using the GCS (modified to the children’s GCS) and a CT scan of the head was obtained to determine the radiologic diagnosis of the injury. The incidence of intracranial hypertension (intracranial pressure [ICP] of >20 mmHg for >5 min) was also noted. Each of the patients was managed using our standard head injury protocol [20], which included placement of an ICP monitor (most often a ventriculostomy) and progressive treatment of intracranial hypertension with sedation, paralysis, cerebrospinal fluid drainage, mild hyperventilation (PaCO2 32–35 Torr), osmotic diuresis, and barbiturates. There were no age-dependent differences in treatment.
Stable XeCT methodology
CBF studies were obtained at the time of admission through post injury day (PID) 9. There was no set schedule for obtaining individual scans in each patient. The XeCT method has been previously described [1] and was used during that 10-year interval as a routine management tool in adults and children after severe TBI [16]. Briefly, the initial head CT scan was obtained using a GE 9800 CT scanner for anatomic diagnosis and localization. Following inhalation of stable Xe gas (33%) and oxygen (67%) for 4.5 min, four CT scans were performed at each of the three standard scanning levels: the first scan localized to pass through the basal ganglia and the mid portion of the third ventricle; the other two levels were obtained 2 cm above and below, respectively.
For each scanning level, a CBF map was then generated with up to 20 contiguous multiple regions of interest (ROIs; 2 cm in diameter) around the cortical mantle, the basal ganglia, and the thalamus bilaterally. CBF was calculated simultaneously using commercially available XeCT CBF software (Diversified Diagnostic Products, Houston, TX) [19, 24]. Regional and hemispheric CBFs were then calculated from the average of all the ROIs within a specific vascular territory or hemisphere and global CBF was defined as the average of all the ROIs. Arterial blood samples obtained prior to each CBF study were analyzed for pH, PaO2, and PaCO2. After obtaining the baseline PaCO2, the end-tidal CO2 was monitored constantly using a capnograph to ensure stability of the PaCO2 throughout the study. No correction of CBF for PaCO2 was performed. Other physiologic parameters including mean arterial pressure and ICP were also recorded.
CO2 vasoreactivity
To determine the responsiveness of CBF to alterations in PaCO2 following TBI, a repeat XeCT study was obtained after altering the tidal volume and/or respiratory rate on the ventilator to change PaCO2 relative to the initial arterial blood gas. A second CBF study was performed at least 15 min after the first and after confirmation of the change in PaCO2 by arterial blood gas measurement. These two-stage studies were used to determine the CO2VR and were obtained in the first 48 h. CO2VR was calculated using the previously defined equation by Obrist et al. [30] which determines the percent change in CBF for each Torr change in PaCO2.
Outcome assessment
Neurological assessment of outcome was determined using the Glasgow Outcome Score (GOS) [18] which we modified for the pediatric age group (Table 1) and was obtained a minimum of 6 months after injury. A final dichotomous outcome was used which categorized patients with either favorable outcome or only moderate disability (GOS 4 or 5) as having “favorable” outcome while those patients who were either severely disabled, vegetative, or who did not survive (GOS ≤3) were categorized as having “unfavorable” outcome.
Statistical analysis
The means and standard deviation (SD) of global and hemispheric CBF and CO2VR were calculated for each study and the results each of the studies were pooled for PID 0, PID 1–2, PID 3–6, PID 7–8, and PID >8 for analysis. Data were also compared between “favorable” and “unfavorable” outcome using a Fisher’s exact test. A Student’s t-test was used to the test the equality of means. A probability value of less than 5% (P < 0.05) was considered significant.
Results
The 95 children included in the study underwent 140 XeCT CBF studies, with 87 of these studies occurring within the first 48 h after admission. There were 69 males and 26 females. The mean age was 8.0 ± 6.1 years, with a range of 0.1–18.4 years. The primary mechanisms of injury included: motor vehicle collision, pedestrian versus motor vehicle, falls, nonaccidental, and recreational injury (bicycle collision). At admission, the average GCS score was 5.9 ± 3.0. Elevated ICP above 20 mmHg and subsequent medication/treatment data was obtained in 86 patients; sustained ICP with aggressive ICP management occurred in 71 of the patients (83%). When refractory intracranial hypertension developed, they were treated as per protocol with escalation of therapy including mannitol (n = 60), addition of Lasix (n = 18), barbiturates (n = 46), and moderate hypothermia (32–33°C) (n = 6) similar to the algorithm delineated subsequently in the Pediatric Guidelines by the author and coauthor [2] and by others [32].
Outcome was evenly split with 47 children having a “favorable” outcome, while 48 of the children had an “unfavorable” outcome. “Unfavorable” outcome was mostly seen in the younger age group (Group I) (76.5%), while the older children (Group II) tended to have less “unfavorable” outcomes (44. 9%).
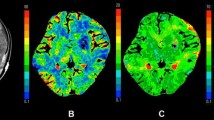
Cerebral blood flow following severe TBI
The mean admission global CBF (PID 0, n = 24) was 32.05 ± 21.45 ml/100 g/min. The mean admission CBF for patients with a “favorable” outcome (n = 11) was 45.64 ± 15.44 ml/100 g/min, while it was 17.85 ± 17.74 ml/100 g/min (P = 0.001) for “unfavorable” outcome (n = 13). At PID 1–2 (n = 61), mean CBF increased to 55.26 ± 23.11 ml/100 g/min; “favorable” outcome (n = 35) was 61.74 ± 18.27 ml/100 g/min; and for “unfavorable” outcome (n = 26), 46.54 ± 26.26 ml/100 g/min (P = 0.010). At PID 3–6, 7–8, and 9, CBF gradually declined to 49.94 ± 22.00, 46.92 ± 17.34, and 42.67 ± 8.72 ml/100 g/min, respectively; with no significant difference in CBF between “favorable” and “unfavorable” outcome groups (Figs. 1, 2 and 3). There was also no difference in CBF between hemispheres on any of the PIDs.
Cerebral blood flow (CBF) measured by xenon CT (XeCT) for all children from post injury day (PID) (admission = 0) through PID 9. CBF is shown as global values, as well as by hemisphere, right (Rt Hemi) and left (Lt Hemi). Note that CBF is initially low at PID 0, subsequently peaking at PID 1–2 post-TBI
Cerebral blood flow (CBF) stratified by outcome (favorable vs. unfavorable) for each interval post injury day (PID). Unfavorable outcome is defined by a Glasgow Outcome Score (GOS) <3, and favorable outcome by a GOS ≥3. Patients with a CBF <20 ml/100 g/min on PID 0–2 had significantly more unfavorable outcomes and patients with CBF >50 ml/100 g/min on PID 0–2 had significantly more favorable outcomes. This trend continued on PID 3–9 but was not significant
For Group I, mean CBF on PID 0 was35.27 ± 21.91 ml/100 g/min and significantly differed between “favorable” (n = 7; 42.92 ± 18.75 ml/100 g/min) and “unfavorable” outcome (n = 5; 12.93 ± 20.75 ml/100 g/min; P = 0.042). Similarly, “favorable” and “unfavorable” outcome mean CBF significantly differed on PID 1–2 (n = 14; 69.31 ± 20.57 ml/100 g/min and n = 15; 40.43 ± 28.77 ml/100 g/min; P = 0.006), respectively. After PID 2, no significant differences were noted in this younger age group (Group I) comparing outcomes (Fig. 4). For the older age group (Group II), a significant difference in mean CBF was only seen at PID 0: “favorable” outcome (n = 4; 50.39 ± 6.70 ml/100 g/min) and “unfavorable” outcome (n = 8; 20.93 ± 16.30 ml/100 g/min (P = 0.011)). All days after this showed no significant difference (Fig. 5).
All patients with a mean CBF <20 ml/100 g/min on PID 0 had an “unfavorable” outcome, while all patients with mean CBF >50 ml/100 g/min had a “favorable” outcome. For PID 1–2, patients with mean CBF <20 ml/100 g/min had significantly less favorable outcome, while patients with CBF >50 ml/100 g/min had significantly better outcome (P = 0.027) (Table 2). For children <5 years, at PID 0 “unfavorable” outcomes only occurred in children with CBF <20 ml/100 g/min and “favorable” outcomes only occurred with CBF >50 ml/100vg/min (P = 0.023). For PID 1–2, of the children with favorable outcomes, 85.71% had a CBF >50 ml/100 g/min (P = 0.023) (Table 3). The older children followed these same trends, but differences did not approach significance. For children <5 years, CBF <20 ml/100 g/min at PID 0 predicted “unfavorable” outcomes with a sensitivity of 1.00 and a specificity of 0.80. Similarly, CBF > 50 ml/100 g/min for PID 1–2 predicted “favorable” outcome with sensitivity 0.86 and specificity 0.67.
There were no significant differences in hematocrit, mean arterial pressure, or PaCO2 between “favorable” and “unfavorable” outcome groups for all patients, and in all age groups (Table 4). Also, there were no significant differences in CBF, hematocrit, mean arterial pressure, or PaCO2 in evaluating mechanism of injury.
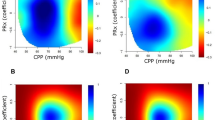
CO2 vasoreactivity
Thirty-eight patients underwent a total of 45 two-stage studies of CO2VR of cerebral circulation, of which 29 studies were obtained in the first 48 h post-TBI. The mean CO2VR was 2.10 ± 8.55 (median 2.59)%/Torr change in PaCO2. Seventeen patients had “favorable” outcomes (20 studies) and 21 had “unfavorable” outcome (25 studies); with mean CO2VR of 3.83 ± 5.70 (median 3.38) and 0.72 ± 10.20 (median 1.84)%/Torr change in PaCO2, respectively P = 0.120 (Fig. 6). In all patients, a lower CO2VR (less than 2%) was associated with a unfavorable outcome (P = 0.086). There was marked variability in response particularly after the first 48 h and for patients with an “unfavorable” outcome. In the evaluation of CO2 autoregulation just within the acute period (the first 48 h after injury), higher mean CO2VR values tended toward a more favorable outcome (“favorable” outcome: 2.95 ± 1.67 (median 3.29)% vs. “unfavorable” outcome: 0.14 ± 8.07 (median 1.58)%/Torr change in PaCO2; P = 0.138), and 64.3% of unfavorable outcome patients had a CO2VR <2%, while only 20% of favorable outcome patients had a CO2VR <2%; P = 0.029 (Fig. 7). There was no correlation between age at injury and CO2VR.
Global CO2 vasoreactivity (CO 2 VR) in all children less than 48 h posttraumatic brain injury (TBI), separated into favorable vs. unfavorable outcomes. Patients with CO2VR <2%/Torr change in PaCO2 have significantly more unfavorable outcomes and patients with CO2VR of 2%–4%/Torr change in PaCO2 have significantly more favorable outcomes (*P < 0.05)
Discussion
At the present time, data from well-designed, controlled studies on acute management of TBI in the pediatric population are sparse and/or lacking. The Guidelines for the Acute Medical Management of Severe Traumatic Brain Injury in Infants, Children, and Adolescents [2] reviewed the literature in this field and showed that there was a lack of understanding as to the physiologic response of the injured pediatric brain as did others [32]. The present study is the largest to evaluate the cerebrovascular response of children following TBI. Using the XeCT technique, we were able to study acute changes in CBF and CO2VR and demonstrate that following pediatric TBI: (1) CBF is initially low, on PID 0, becomes elevated on PID 1–2, and then equalizes after PID 3 but; (2) early low CBF, and CBF <20 ml/100 g/min, were correlated with a unfavorable outcome; (3) early higher CBF and CBF >50 ml/100 g/min was correlated with a favorable outcome; and (4) loss of CO2VR (≤2%/Torr change PaCO2) within the first 48 h of injury was associated with an unfavorable outcome.
Cerebrovascular response after pediatric TBI
As a whole, children tend to have lower morbidity and mortality versus adults; however, infants and younger children (<5 years old) tend to have less favorable outcomes after TBI [23]. Because there is a lack of studies on this subgroup, it is unclear whether this difference is due to mechanism of injury or the age related anatomy and physiology/pathophysiologic processes in response to the injury of these younger children. Uniquely, and most importantly, especially in this larger series, was our finding that early low CBF was significantly associated with an unfavorable outcome. Low CBF was seen across all groups in the first 24 h following TBI but was significantly lower in unfavorable outcome groups, across all ages. Furthermore, for children <5 years; those with “unfavorable” outcome also had a significantly lower CBF on PID 1–2 indicating the potential importance of CBF promoting strategies to aid in the recovery phase in this young age group. For all children, a CBF ≤20 ml/100 g/min at any point was correlated with a unfavorable outcome, suggesting a critical level of CBF may be needed even in the acute period, though whether this finding represents a treatment goal or prognostic indicator remains to be determined. Early hypoperfusion and the relationship of early low CBF and outcome after TBI observed in our study mirrors those of similar studies in adults [8, 9, 24].
Previous studies of cerebrovascular response in adults [9, 14, 24, 28–30] and older children [26, 27, 33] after TBI showed a trend that low CBF within 24 h of injury may be associated with “unfavorable” outcomes and high CBF during this time has no effect on outcome. These studies were important in understanding the changes in CBF in response to TBI, however few infants and young children were included in these studies. Using the 133Xe method, Bruce et al. [10, 11] studied TBI patients that were between 16 and 21 years and suggested that the mechanism underlying the “malignant” cerebral swelling often found in children post-TBI was an age related hyperemia. Brain swelling was previously believed to be due to “vasomotor paralyses” and increased cerebral blood volume (CBV) and not edema [15]. The seminal work by Marmarou et al. [25], using magnetic resonance imaging techniques in adults, suggests a heterogeneous response after TBI. Cytotoxic edema and reduced CBV occurred in the majority of adults during the initial 7 days after severe TBI, though normal and increased CBV occurred in a subset of patients who developed secondary cerebral swelling.
Again using 133Xe method, Kasoff et al. [19] reported on CBF in ten children in the acute period at various times after injury. The children were ages 9 months to 12 years, with a mean age of 7 years. In that study, six of the children had regional increases in CBF, 2–5 times normal flow that were interpreted as hyperperfusion but not related to age. Using the nitrous oxide method, Sharples et al. [33] reported on 21 children (ages 2–16 years) with an average age of 6 years, but with only five children <4 years, and showed that mean CBF was higher in children soon after TBI in favorable outcome groups; and 24 h after injury global CBF did not vary between favorable and unfavorable outcome groups. In a preliminary report using the 133Xe method, Beyda [7] found that initially low CBFs became hyperemic by PID 3 after TBI, which he proposed to represent delayed uncoupling of CBF and oxidative metabolism, as seen in adults [29, 30]. Also, he noticed that ICP peaked at this time, suggesting that there is a relationship between CBF and ICP. All of these studies were very limited in scope in terms of studying young children. Using the 133Xe method, Muizelaar et al. [ 26, 27] studied 32 children following TBI, but the mean age was 14 and only four children were <8 years. He showed that lower CBF values in children immediately after TBI correlated with a unfavorable outcome. We published a preliminary report on 33 children <8 years of age using the XeCT method and, combined with our present study, represents the largest series of CBF data in young children and infants after TBI, with 44 children <5 years of age. Younger children (particularly those <2 years) tended to have poorer outcomes than older children but again was only small numbers. Similar outcomes for infants and young children from our study and those of Aldrich et al. [3] help validate and generalize the CBF findings in this subgroup of patients.
CBF and “hyperemia”
The relationship between posttraumatic “hyperemia,” diffuse cerebral swelling, and intracranial hypertension remains in question in children after severe TBI. Because children more commonly develop diffuse cerebral swelling than adults [3, 4, 37], it has been suggested since the initial work of Bruce et al. [10, 11] that this is an age related hyperemia.
In this study, patients from all age groups with “favorable” outcome had significantly higher CBF immediately post-TBI (PID 0) when compared to patients with “unfavorable” outcome. This was particularly true in children <5 years of age where CBF ≥50 ml/100 g/min at PID 1–2 was correlated with significantly better outcomes and exhibited both high sensitivity and specificity for predicting the favorable long-term outcomes. Mean CBF for these children was >55 ml/100 g/min as compared to those with “unfavorable” outcome, where mean CBF was ~40 ml/100 g/min. One possibility is that young children represent a particularly sensitive group, in which maintenance of normal levels of CBF immediately after injury through the first 2 days post TBI may be critical for adequate recovery. The mean CBF in this age group is higher than the mean CBF reported in adults during this time period (45 ml/100 g/min) [37] though this may represent the “normal” or adequate CBF in this younger age population indicating that disturbance in normal CBF may be more indicative of outcome than elevated CBF values. Similarly, any comparisons and differences must take into consideration both the differences in methodology when trying to determine normal CBF in these different age groups. Chiron et al. [12] used 133Xe SPECT and reported that CBF starts at 50 ml/100 g/min in normal neonates, rises to 71 ml/100 g/min in children ages 6–8 years, and then declines to adult levels. In any case, our findings suggest that early low CBF, particularly in infants and young children, may represent an important therapeutic or prognostic target (ischemia) – and this represents a major departure from traditional dogma on pediatric TBI that results in hyperemia. However, we cannot rule out a coupled reduction of CBF and cerebral metabolic rate (CMR) given the absence of concomitant data on CMR.
CO2VR after pediatric TBI
In the work by Obrist et al. [30], normal CO2VR was 3 ± 1% change in CBF/Torr change in PaCO2. Cold et al. [13] reported that CO2VR was low, ~1.9%, after TBI versus normative data in adults. Enevoldsen and Jensen [14] reported that normal CO2VR was lost after severe TBI, particularly in patients with severe injuries where they considered a value of ≤2% as abnormal. Some children as young as 6 years were included but no separate analysis was performed for this younger age group. In this study, disturbed CO2 VR in pediatric TBI with “normal” autoregulation in the first 48 h correlated with a favorable outcome though there were only a small number of patients studied for both parameters. However, this significant difference in outcomes according to CO2VR is not seen in studies done after 48 h post injury possibly due to small sample size and regional heterogeneity. Further data on CO2 VR in infants and children after TBI are needed to determine the predictive value of CO2 VR and outcome.
CBF values in most previous studies were normalized to a PaCO2 of 34 mmHg by assuming a CO2VR of 3% [14, 28, 30, 31]. The validity of this technique remains in question since prolonged hyperventilation may change CO2VR [30, 37] and CO2VR may be impaired. In this study, CBF was not normalized to PaCO2 and we found there was significant variability of CO2VR between and within outcome groups in the acute post trauma period. Whether this is true variability and or whether it is valid to normalize for low CO2 remains in question and would also need to be addressed prospectively in future studies.
Limitations
Our study is limited by statistical and clinical considerations. This was a retrospective study that collected data over a 10-year period from patients managed from a decade ago. While there have been more defined management protocols in the interim, unfortunately not much has changed in how patients were managed during that time period as compared to today. Much of the management used by the authors [20] was based on the literature that was eventually included in the Pediatric Guidelines [2]. This though should not take away from the findings since no correlations were made between the specific clinical management and the clinical parameters for each of the different age at injury and outcomes groups. We cannot rule out the possibility that management lead to differences in CBF and autoregulatory response. However, low CBF often was seen early after TBI, prior to the measurement and treatment of intracranial pressure. For the most part though, the clinical management conformed to the Pediatric Guidelines [2] except these patients predated the use of hypothermia that is now being tested by the author in a clinical trial.
Another limitation is that XeCT CBF monitoring is no longer performed in children with stable Xe being reevaluated for potential negative effects by the FDA in the United States (H. Yonas, personal communication). The FDA requested additional safety data on this test and this method is again available for research use but has mostly been used in adults. Also, there have never been any established protocols for the time points in which to perform XeCT CBF monitoring after severe TBI in children. As a result, not all children received studies at all the time points that we studied. A prospective protocol with defined time of imaging would provide better understanding of the cerebrovascular response in children at these different time points. Correlation with CSF, urine or serum biomarkers and known mediators of CBF is also warranted [5, 6, 21].
Lastly, ≥24 h after TBI in infants and young children, there was significant heterogeneity between individual patients both in response and outcome. For example, a CBF of 78 ml/100 g/min PID 1–2 in a 4-year-old child in our study with only mild hypoperfusion on admission, modest intracranial hypertension, intact CO2VR, and favorable outcome; almost certainly represents recovery of normal CBF. In contrast, a 2-month-old infant in our study presented with a CBF of only 9 ml/100 g/min at admission but had a CBF of 58 ml/100 g/min at 24 h post injury. This child though had minimal CO2VR, refractory intracranial hypertension, and ultimately died; probably represents an initial “ischemic” insult followed by a “hyperemic” response with loss of cerebral autoregulation. However, since concurrent measures of metabolic demand were not obtained, the marked elevation of the CBF in this patient should not be termed “hyperemia” and was not addressed by our study. In these patients, the pathologic response may or may not be temporarily coupled to intracranial hypertension. Further physiologic data as to cerebral metabolic demand is needed. In addition, there were insufficient numbers of children <2 years of age to make any real age comparisons and while this subgroup may have particular susceptibility, further studies are necessary. These examples highlight the heterogeneity of outcome and response to injury following TBI regardless of age and provide impetus for not only better understanding but the need for more neurophysiologic monitoring to better guide individualized care.
Conclusion
This report represents the largest study of CBF focusing on children and infants after TBI. Patients with a low global CBF ≤20 ml/100 g/min, following TBI were significantly associated with “unfavorable” outcomes. Higher CBF (≥50 ml/100 g/min) in patients on PID 0 and 1–2 days post-TBI in children <5 years was associated with “favorable” outcomes. This could represent either preservation of a normal physiologic or pathophysiologic response to TBI in young children with favorable outcome and/or a potential therapeutic goal for this age group. Impaired cerebral autoregulation, CO2VR <2%, within 48 h of injury was associated with an “unfavorable” outcome and may need to be taken into consideration when managing this patient population. Lastly, further study prospectively and with multimodality monitoring is encouraged to better define the complex cerebrovascular response in children following TBI.
References
Adelson PD, Clyde B (1997) Cerebrovascular response in infants and young children following severe traumatic brain injury: A preliminary report. Pediatr Neurosurg 26:200–2007
Adelson PD, Bratton SL, Carney NA, Chesnut RM, du Coudray HE, Goldstein B, Kochanek PM, Miller HC, Partington MD, Selden NR, Warden CR, Wright DW (2003) Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Pediatr Crit Care Med 4(3 Suppl):S2–75
Aldrich EF, Eisenberg HM, Saydjari C, Luerssen TG, Foulkes MA, Jane JA, Marshall LF, Marmarou A, Young HF (1992) Diffuse brain swelling in severely head-injured children. A report from the NIH Traumatic Coma Data Bank. J Neurosurg 76:450–454
Berger MS, Pitts LH, Lovely M, Edwards MS, Bartkowski HM (1985) Outcome from severe head injury in children and adolescents. J Neurosurg 62:194–199
Berger RP, Kochanek PM (2006) Urinary S100B concentrations are increased after brain injury in children: A preliminary study. Pediatr Crit Care Med 7:557–556
Berger RP, Adelson PD, Richichi R, Kochanek PM (2006) Serum biomarkers after traumatic and hypoxemic brain injuries: Insight into the biochemical response of the pediatric brain to inflicted brain injury. Dev Neurosci 28(4–5):327–335
Beyda DH (1996) Time course of cerebral blood flow and metabolism in pediatric head trauma (abstract). Crit Care Med 24:134
Bouma GJ, Muizelaar JP, Choi SC, Newlon PG, Young HF (1991) Cerebral circulation and metabolism after severe traumatic brain injury: the elusive role of ischemia. J Neurosurg 75:685–693
Bouma GJ, Muizelaar JP, Stringer WA, Choi SC, Fatouros P, Young HF (1992) Ultra-early evaluation of regional cerebral blood flow in severely head-injured patients using xenon-enhanced computerized tomography. J Neurosurg 77:360–368
Bruce DA, Schut L, Bruno LA, Wood JH, Sutton LN (1978) Outcome following severe head injury in children. J Neurosurg 48:679–688
Bruce DA, Alavi A, Bilaniuk LT, Dolinskas C, Obrist W, Uzzell B (1981) Diffuse cerebral swelling following head injuries in children: The syndrome of ‘malignant brain edema’. J Neurosurg 54:170–178
Chiron C, Raynaud C, Maziere B, Zilbovicius M, Laflamme L, Masure M-C, Dulac O, Bourguignon M, Syrota A (1992) Changes in regional cerebral blood flow during brain maturation in children and adolescents. J Nucl Med 33:696–703
Cold GE, Jensen FT, Malmros R (1977) The cerebrovascular CO2 reactivity during the acute phase of brain injury. Acta Anaesthesiol Scand 21:222–231
Enevoldsen EM, Jensen FT (1978) Autoregulation and CO2 responses of cerebral blood flow in patients with acute severe head injury. J Neurosurg 48:689–703
Ewing-Cobbs L, Miner ME, Fletcher JM, Levin HS (1989) Intellectual, motor, and language sequelae following closed head injury in infants and preschoolers. J Pediatr Psychol 14:531–547
Gur D, Yonas H, Good WF (1989) Local cerebral blood flow by Xenon-Enhanced CT: Current status, potential improvements and future directions. Cerebrovasc Brain Metab Rev 1:68–86
Jankowitz BT, Adelson PD (2006) Pediatric traumatic brain injury: Past, present, and future. Dev Neurosci 28(4–5):264–75
Jennett B, Bond M (1985) Assessment of outcome after severe brain damage. Lancet i:480–484
Kasoff SS, Zingesser LH, Shulman K (1972) Compartmental abnormalities of regional cerebral blood flow in children with head trauma. J Neurosurg 36:463–470
Kochanek PK, Clark RSB, Adelson PD, Marion DW (1995) Severe traumatic brain injury in children: Pathobiology, management, and controversies; in Green TP, Weigle CGM (eds): Current Concepts in Pediatric Critical Care. Fullerton, Soc of Crit Care Med
Kochanek PM, Clark RSB, Ruppel RA, Adelson PD, Bell MJ, Whalen MJ, Robertson CL, Satchell MA, Seidberg NA, Marion DW, Jenkins LW (2000) Biochemical, cellular and molecular mechanisms in the evolution of secondary damage after severe traumatic brain injury in infants and children: Lessons learned from the bedside. Pediatr Crit Care Med 1:4–19
Levin HS, Eisenberg HM, Wigg NR, Kobayashi K (1982) Memory and intellectual ability after head injury in children and adolescents. Neurosurgery 11:668–673
Luersen TG, Klauber MR, Marshall LF (1988) Outcome from head injury related to patient’s age: A longitudinal prospective study of adult and pediatric head injury. J Neurosurg 68:409–416
Marion DW, Darby J, Yonas H (1991) Acute regional cerebral blood flow changes caused by severe heas injuries. J Neurosurg 74:407–414
Marmarou A, Barzo P, Fatouros P, Yamamoto T, Doppenberg E, Muizelaar P, Bullock R, Young H (1996) Traumatic brain swelling in head injured patients: Brain edema or vascular engorgement? Proc 10th Int Brain Edema Symp, p 90
Muizelaar JP, Ward JD, Marmarou A, Newlon PG, Wachi A (1989) Cerebral blood flow and metabolism in severely head-injured children: II. Autoregulation. J Neurosurg 71:72–76
Muizelaar JP, Marmarou A, DeSalles AAF, Ward JD, Zimmerman RS, Li Z, Choi SC, Young HF (1989) Cerebral blood flow and metabolism in severely head-injured children. I: Relationship with GCS score, outcome, ICP, and PVI. J Neurosurg 71:63–71
Muizelaar JP, Marmarou A, Ward JD, Kontos HA, Choi SC, Becker DP, Gruemer H, Young HF (1991) Adverse effects of prolonged hyperventilation in patients with severe head injury: A randomized clinical trial. J Neurosurg 75:731–739
Obrist WD, Marion DW, Aggarwal S, Darby JM (1993) Time course of cerebral blood flow and metabolism in comatose patients with acute head injury. J Cereb Blood Flow Metab 13(suppl):571
Obrist WD, Langfitt TW, Jaggi JL, Cruz J, Gennarelli TA (1984) CBF and metabolism in comatose patients with acute head injury. J Neurosurg 61:241–253
Overgaard J, Tweed WA (1974) Cerebral circulation after head injury. I: Cerebral blood flow and its regulation after closed head injury with emphasis on clinical correlations. J Neurosurg 41:531–541
Pietrini D, Savioli A, Grossetti R, Barbieri MA, Buscalferri A, Calamandrei M, Chiaretti A, David A, Di Rocco C, Dusio MP, Febi G, Gallini C, Giordano F, Girasole V, Lampugnani E, Laviani Mancinelli R, Levati A, Mazza C, Meneghini L, Paccagnella F, Piastra M, Procaccini E, Pusateri A, Scielzo R, Stofella G, Stoppa F, Tamburrini G, Testoni C, Tumolo M, Velardi F, Zei E, Latronico N (2004) SIAARTI-SARNePI Guidelines for the management of severe pediatric head injury. Minerva Anestesiol 70(7–8):545–547
Sharples PM, Stuart AG, Matthews DSF, Aynsely-Green A, Eyre JA (1995) Cerebral blood flow and metabolism in children with severe head injury: I. Relation to age, glasgow coma score, outcome, intracranial pressure, and time after injury. J Neurol Neurosurg Psychiatry 58:145–152
Vavilala MS, Lee LA, Boddu K, Visco E, Newell DW, Zimmerman JJ, Lam AM (2004) Cerebral autoregulation in pediatric traumatic brain injury. Pediatr Crit Care 5(3):257–263
Vavilala MS, Muangman S, Tontisirin N, Fisk D, Roscigno C, Mitchell P, Kirkness C, Zimmerman JJ, Chestnut R, Lam AM (2006) Impaired cerebral autoregulation and 6-month outcome in children with severe traumatic brain injury: Preliminary findings. Dev Neurosci 28(4–5):348–53
Vavilala MS, Muangman S, Waitayawinyu P, Roscigno C, Jaffe K, Mitchell P, Kirkness C, Zimmerman JJ, Ellenbogen R, Lam AM (2007) Impaired cerebral autoregulation in infants and young children early after inflicted traumatic brain injury: A preliminary report. J Neurotrauma 24:87–96
Zimmerman RA, Bilaniuk LT, Bruce D (1978) Computed tomography of pediatric head trauma. Radiology 126:403–408
Acknowledgements
The authors would like to thank Ms. Christina Casanova for the preparation of this manuscript and S. Danielle Brown, MSN, who served as the honest broker. The author (PDA) was supported in part for this study by the National Institute of Health (NS01809, NS052478). The authors have no personal or institutional financial interest in drugs, materials, or devices described in this submission.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Adelson, P.D., Srinivas, R., Chang, Y. et al. Cerebrovascular response in children following severe traumatic brain injury. Childs Nerv Syst 27, 1465–1476 (2011). https://doi.org/10.1007/s00381-011-1476-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-011-1476-z