Abstract
Purpose
To assess the feasibility, safety, and outcomes of an expedited One-Stop prostate cancer (PCa) diagnostic pathway.
Patients and methods
We identified 370 consecutive patients who underwent multiparametric magnetic resonance imaging (mpMRI) and transrectal ultrasound fusion prostate biopsy (MRI/TRUS-PBx) from our institutional review board-approved database. Patients were divided according to diagnostic pathway: One-Stop (n = 74), with mpMRI and same-day PBx, or Standard (n = 296), with mpMRI followed by a second visit for PBx. mpMRIs were performed and interpreted according to Prostate Imaging-Reporting and Data System (PI-RADS v2). Grade group ≥ 2 PCa defined clinically significant PCa (csPCa). Statistical significance was considered when p < 0.05.
Results
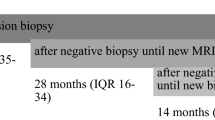
Age (66 vs 66 years, p = 0.59) and PSA density (0.1 vs 0.1 ng/mL2, p = 0.26) were not different between One-Stop vs Standard pathway, respectively. One-Stop patients lived further away from the hospital than Standard patients (163 vs 31 km; p < 0.01), and experienced shorter time from mpMRI to PBx (0 vs 7 days; p < 0.01). The number (p = 0.56) and distribution of PI-RADS lesions (p = 0.67) were not different between the groups. All procedures were completed successfully with similar perioperative complications rate (p = 0.24). For patients with PI-RADS 3–5 lesions, the csPCa detection rate (49% vs 41%, p = 0.55) was similar for One-Stop vs Standard, respectively. The negative predictive value of mpMRI (PI-RADS 1–2) for csPCa was 78% for One-Stop vs 83% for Standard (p = 0.99). On multivariate analysis, age, prostate volume and PI-RADS score (p < 0.01), but not diagnostic pathway, predicted csPCa detection.
Conclusion
A One-Stop PCa diagnostic pathway is feasible, safe, and provides similar outcomes in a shorter time compared to the Standard two-visit diagnostic pathway.

Similar content being viewed by others
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- AS:
-
Active surveillance
- CI:
-
Confidence interval
- csPCa:
-
Clinically significant prostate cancer
- DCE:
-
Dynamic contrast-enhanced
- DRE:
-
Digital rectal examination
- DWI:
-
Diffusion-weighted images
- IQR:
-
Interquartile range
- ISUP:
-
International Society of Urological Pathology
- mpMRI:
-
Multiparametric magnetic resonance imaging
- MRI/TRUS-PBx:
-
Magnetic resonance imaging transrectal ultrasound fusion-guided prostate biopsy
- NPV:
-
Negative predictive value
- OR:
-
Odds ratio
- PBx:
-
Prostate biopsy
- PCa:
-
Prostate cancer
- PI-RADS v.2:
-
Prostate Imaging-Reporting and Data System Version 2
- PPV:
-
Positive predictive value
- PSA:
-
Prostatic specific antigen
- UTI:
-
Urinary tract infection
References
Kasivisvanathan V, Rannikko AS, Borghi M, Panebianco V, Mynderse LA, Vaarala MH et al (2018) MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med 378(19):1767–1777
Singh M, Maheu C, Brady T, Farah R (2017) The psychological impact of the rapid diagnostic centres in cancer screening: a systematic review. Can Oncol Nurs J 27(4):348–355
Berg WT, Danzig MR, Pak JS, Korets R, RoyChoudhury A, Hruby G et al (2015) Delay from biopsy to radical prostatectomy influences the rate of adverse pathologic outcomes. Prostate 75(10):1085–1091
Weinreb JC, Barentsz JO, Choyke PL, Cornud F, Haider MA, Macura KJ et al (2016) PI-RADS prostate imaging-reporting and data system: 2015, version 2. Eur Urol 69(1):16–40
Oishi M, Shin T, Ohe C, Nassiri N, Palmer SL, Aron M, Ashrafi AN, Cacciamani GE, Chen F, Duddalwar V, Stern MC, Ukimura O, Gill IS, Luis de Castro Abreu A (2019) Which patients with negative magnetic resonance imaging can safely avoid biopsy for prostate cancer? J Urol 201(2):268–277. https://doi.org/10.1016/j.juro.2018.08.046
Liss MA, Ehdaie B, Loeb S, Meng MV, Raman JD, Spears V et al (2017) An update of the American Urological Association white paper on the prevention and treatment of the more common complications related to prostate biopsy. J Urol 198(2):329–334
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA, The 2014 International Society of Urological Pathology (ISUP) (2016) Consensus conference on gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol 40(2):244–252
Ahmed HU, Bosaily AE-S, Brown LC, Gabe R, Kaplan R, Parmar MK et al (2017) Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 389(10071):815–822
Wegelin O, Exterkate L, van der Leest M, Kummer JA, Vreuls W, de Bruin PC, Bosch JLHR, Barentsz JO, Somford DM, van Melick HHE (2019) The FUTURE trial: a multicenter randomised controlled trial on target biopsy techniques based on magnetic resonance imaging in the diagnosis of prostate cancer in patients with prior negative biopsies. Eur Urol 75(4):582–590. https://doi.org/10.1016/j.eururo.2018.11.040
Bass EJ, Freeman A, Jameson C, Punwani S, Moore CM, Arya M et al (2018) Prostate cancer diagnostic pathway: is a one-stop cognitive MRI targeted biopsy service a realistic goal in everyday practice? A pilot cohort in a tertiary referral centre in the UK. BMJ Open 8(10):e024941
Oberlin DT, Casalino DD, Miller FH, Meeks JJ (2017) Dramatic increase in the utilization of multiparametric magnetic resonance imaging for detection and management of prostate cancer. Abdom Radiol (N Y) 42(4):1255–1258
Fossati N, Rossi MS, Cucchiara V, Gandaglia G, Dell'Oglio P, Moschini M, Suardi N, Dehò F, Montorsi F, Schiavina R, Mottrie A, Briganti A (2017) Evaluating the effect of time from prostate cancer diagnosis to radical prostatectomy on cancer control: can surgery be postponed safely? Urol Oncol 35(4):150.e9–150.e15. https://doi.org/10.1016/j.urolonc.2016.11.010
Korets R, Seager CM, Pitman MS, Hruby GW, Benson MC, McKiernan JM (2012) Effect of delaying surgery on radical prostatectomy outcomes: a contemporary analysis. BJU Int 110(2):211–216
Morini MA, Muller RL, de Castro Junior PCB, de Souza RJ, Faria EF (2018) Time between diagnosis and surgical treatment on pathological and clinical outcomes in prostate cancer: does it matter? World J Urol 36(8):1225–1231
Watts S, Leydon G, Birch B, Prescott P, Lai L, Eardley S et al (2014) Depression and anxiety in prostate cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open 4(3):e003901
Jiang P, Liss MA, Szabo RJ (2018) Targeted antimicrobial prophylaxis does not always prevent sepsis after transrectal prostate biopsy. J Urol 200(2):361–368
Xiang J, Yan H, Li J, Wang X, Chen H, Zheng X (2019) Transperineal versus transrectal prostate biopsy in the diagnosis of prostate cancer: a systematic review and meta-analysis. World J Surg Oncol 17(1):31
Grummet JP, Weerakoon M, Huang S, Lawrentschuk N, Frydenberg M, Moon DA et al (2014) Sepsis and ‘superbugs’: should we favour the transperineal over the transrectal approach for prostate biopsy? BJU Int 114(3):384–388
Loeb S, Vellekoop A, Ahmed HU, Catto J, Emberton M, Nam R et al (2013) Systematic review of complications of prostate biopsy. Eur Urol 64(6):876–892
Borghesi M, Ahmed H, Nam R, Schaeffer E, Schiavina R, Taneja S et al (2017) Complications after systematic, random, and image-guided prostate biopsy. Eur Urol 71(3):353–365
Pinkhasov GI, Lin YK, Palmerola R, Smith P, Mahon F, Kaag MG et al (2012) Complications following prostate needle biopsy requiring hospital admission or emergency department visits—experience from 1000 consecutive cases. BJU Int 110(3):369–374
Nilbert M, Bläckberg M, Ceberg J, Hagberg O, Stenhoff R, Liedberg F (2018) Diagnostic pathway efficacy for urinary tract cancer: population-based outcome of standardized evaluation for macroscopic haematuria. Scand J Urol 52(4):237–243. https://doi.org/10.1080/21681805.2018.1498124
Safir IJ, Gabale S, David SA, Huang JH, Gerhard RS, Pearl J et al (2016) Implementation of a tele-urology program for outpatient hematuria referrals: initial results and patient satisfaction. Urology 97:33–39
Acknowledgements
This study was funded by the R01 Grant CA205058-01 from the National Institutes of Health/National Cancer Institute (M. C. S, I. S. G. and A. L. D. C. A.) and in part by the Australasian Urological Foundation Scholarship (A. N. A).
Author information
Authors and Affiliations
Contributions
AA, AT, ANA, SP: project development, analysis interpretation, manuscript writing. AS: data collection, manuscript writing and language revision. JC: statistical analysis. AI, TI, AS, CG, LGM: data collection. GEC: data collection and analysis interpretation. MCS, VD, MA, ISG: other (supervision and critical revision).
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. This study was funded by the R01 Grant CA205058-01 from the National Institutes of Health/National Cancer Institute (M. C. S, I. S. G. and A. A.) and in part by the Australasian Urological Foundation Scholarship (A. N. A). Dr. Vinay Duddalwar is a consultant for Intuitive Surgical and Radmetrix, sits on the advisory board for DeepTek, and received grant support from Samsung Healthcare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tafuri, A., Ashrafi, A.N., Palmer, S. et al. One-Stop MRI and MRI/transrectal ultrasound fusion-guided biopsy: an expedited pathway for prostate cancer diagnosis. World J Urol 38, 949–956 (2020). https://doi.org/10.1007/s00345-019-02835-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02835-2