Abstract
Objectives
This study aimed to evaluate the value of nodal grouping (NG), defined as the presence of at least three contiguous lymph nodes (LNs) within one LN region, in staging and management of patients with non-metastatic nasopharyngeal carcinoma (NPC).
Methods
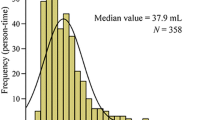
MR images were reviewed to evaluate LN variables, including NG. The Kaplan–Meier method and multivariate Cox regression models evaluated the association between the variables and survival. Harrell’s concordance index (C-index) was used to measure the performance of prognostic models. The outcome of induction chemotherapy (IC) in patients with and without NG was compared using matched-pair analysis.
Results
In 1224 patients enrolled, NG was found to be an independent prognostic factor for overall survival (OS), progression-free survival (PFS), distant metastasis-free survival (DMFS), and regional recurrence-free survival. The hazard ratio and 95% confidence interval (CI) of NG for OS (3.86, 2.09–7.12) were higher than those of stage N2 (3.54, 1.89–6.70). On upgrading patients with NG from stages N1 to N2, the revised N staging yielded a higher C-index compared to the American Joint Committee on Cancer system in predicting PFS (0.664 vs. 0.658, p = 0.022) and DMFS (0.699 vs. 0.690, p = 0.005). Results of the matched-pair analysis revealed that for patients with NG in stages N1 and N2, IC was correlated with improved OS (p = 0.022), PFS (p = 0.007), and DMFS (p = 0.021).
Conclusions
NG is a significant prognostic factor for patients with NPC. Patients with NG may be upgraded from stages N1 to N2. NG was also a marker for identifying patients who would benefit from IC.
Key Points
• Nodal grouping, defined as the presence of at least three contiguous LNs within one LN region on MRI, was identified as a significant prognostic factor.
• In patients with nasopharyngeal carcinoma, nodal grouping may influence lymph node staging.
• Nodal grouping was a marker for identifying patients who may benefit from induction chemotherapy.




Similar content being viewed by others
Abbreviations
- AJCC:
-
American Joint Committee on Cancer
- C-index:
-
Harrell’s concordance index
- CCRT:
-
Concurrent chemoradiotherapy
- CI:
-
Confidence interval
- CNN:
-
Central nodal necrosis
- DMFS:
-
Distant metastasis-free survival
- EBV:
-
Epstein–Barr virus
- ENS:
-
Extracapsular nodal spread
- FSE:
-
Fast spin-echo
- HR:
-
Hazard ratio
- IC:
-
Induction chemotherapy
- IMRT:
-
Intensity-modulated radiation therapy
- LN:
-
Lymph node
- MD:
-
Maximal diameter
- MID:
-
Minimal axial diameter
- NG:
-
Nodal grouping
- NPC:
-
Nasopharyngeal carcinoma
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- RRFS:
-
Regional recurrence-free survival
- T1WI :
-
1-weighted images
- T2WI:
-
T2-weighted images
References
Wei WI, Sham JST (2005) Nasopharyngeal carcinoma. Lancet 365:2041–2054
Lai SZ, Li WF, Chen L et al (2011) How does intensity-modulated radiotherapy versus conventional two-dimensional radiotherapy influence the treatment results in nasopharyngeal carcinoma patients. Int J Radiat Oncol Biol Phys 80:661–668
Mao YP, Tang LL, Chen L et al (2016) Prognostic factors and failure patterns in non-metastatic nasopharyngeal carcinoma after intensity-modulated radiotherapy. Chin J Cancer 35:103
Amin MB, Edge SB, Greene FL et al (2016) AJCC cancer staging manual, 8th edn. Springer, New York
Tang LL, Chen YP, Mao YP et al (2017) Validation of the 8th edition of the UICC/AJCC staging system for nasopharyngeal carcinoma from endemic areas in the intensity-modulated radiotherapy era. J Natl Compr Canc Netw 15:913–919
OuYang PY, Xiao Y, You KY et al (2017) Validation and comparison of the 7th and 8th edition of AJCC staging systems for non-metastatic nasopharyngeal carcinoma, and proposed staging systems from Hong Kong, Guangzhou, and Guangxi. Oral Oncol 72:65–72
Yang XL, Wang Y, Liang SB et al (2018) Comparison of the seventh and eighth editions of the UICC/AJCC staging system for nasopharyngeal carcinoma: analysis of 1317 patients treated with intensity-modulated radiotherapy at two centers. BMC Cancer 18:606
Pan JJ, Ng WT, Zong JF et al (2016) Proposal for the 8th edition of the AJCC/UICC staging system for nasopharyngeal cancer in the era of intensity-modulated radiotherapy. Cancer 122:546–558
Groome PA, Schulze K, Boysen M, Hall SF, Mackillop WJ (2001) A comparison of published head and neck stage groupings in carcinoma of the oral cavity. Head Neck 8:613–624
You SH, Kim B, Yang KS, Kim BK (2019) Cervical necrotic lymphadenopathy: a diagnostic tree analysis model based on CT and clinical findings. Eur Radiol 29:5635–5645
Mao YP, Liang SB, Liu LZ et al (2008) The N staging system in nasopharyngeal carcinoma with radiation therapy oncology group guidelines for lymph node levels based on magnetic resonance imaging. Clin Cancer Res 14:7497–7503
Lan M, Huang Y, Chen CY et al (2015) Prognostic value of cervical nodal necrosis in nasopharyngeal carcinoma: analysis of 1800 patients with positive cervical nodal metastasis at MR imaging. Radiology 276:619
Zhang LL, Li JX, Zhou GQ et al (2017) Influence of cervical node necrosis of different grades on the prognosis of nasopharyngeal carcinoma patients treated with intensity-modulated radiotherapy. J Cancer 8:959–966
Maxwell JH, Ferris RL, Gooding W et al (2013) Extracapsular spread in head and neck carcinoma: impact of site and human papillomavirus status. Cancer 119:3302–3308
van den Brekel MW, Stel HV, Castelijns JA et al (1990) Cervical lymph node metastasis: assessment of radiologic criteria. Radiology 177:379–384
Zhang GY, Liu LZ, Wei WH, Deng YM, Li YZ, Liu XW (2010) Radiologic criteria of retropharyngeal lymph node metastasis in nasopharyngeal carcinoma treated with radiation therapy. Radiology 255:605–612
Wan Y, Tian L, Zhang G et al (2019) The value of detailed MR imaging report of primary tumor and lymph nodes on prognostic nomograms for nasopharyngeal carcinoma after intensity-modulated radiotherapy. Radiother Oncol 131:35–44
Shao JY, Zhang Y, Li YH et al (2004) Comparison of Epstein-Barr virus DNA level in plasma, peripheral blood cell and tumor tissue in nasopharyngeal carcinoma. Anticancer Res 24:4059–4066
R Core team: R: a language and environment for statistical computing. R foundation for statistical computing, R foundation for statistical computing, available at: https://www.R-project.org
Ahmad A, Reha J, Saied A, Espat NJ, Somasundar P, Katz SC (2017) Association of primary tumor lymph node ratio with burden of liver metastases and survival in stage IV colorectal cancer. Hepatobiliary Surg Nutr 6:154–161
Ho AS, Kim S, Tighiouart M et al (2018) Association of quantitative metastatic lymph node burden with survival in hypopharyngeal and laryngeal cancer. JAMA Oncol 4:985–989
Ho AS, Kim S, Tighiouart M et al (2017) Metastatic lymph node burden and survival in oral cavity cancer. J Clin Oncol 35:3601–3609
Ebrahimi A, Gil Z, Amit M et al (2014) The prognosis of N2b and N2c lymph node disease in oral squamous cell carcinoma is determined by the number of metastatic lymph nodes rather than laterality: evidence to support a revision of the American Joint Committee on Cancer staging system. Cancer 120:1968–1974
Shaw RJ, Lowe D, Woolgar JA et al (2010) Extracapsular spread in oral squamous cell carcinoma. Head Neck 32:714–722
Sun Y, Li WF, Chen NY et al (2016) Induction chemotherapy plus concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in locoregionally advanced nasopharyngeal carcinoma: a phase 3, multicentre, randomised controlled trial. Lancet Oncol 17:1509–1520
Ribassin-Majed L, Marguet S, Lee AWM et al (2017) What is the best treatment of locally advanced nasopharyngeal carcinoma? An individual patient data network meta-analysis. J Clin Oncol 35:498–505
Hong RL, Ting LL, Ko JY et al (2001) Induction chemotherapy with mitomycin, epirubicin, cisplatin, fluorouracil, and leucovorin followed by radiotherapy in the treatment of locoregionally advanced nasopharyngeal carcinoma. J Clin Oncol 19:4305–4313
Fountzilas G, Ciuleanu E, Bobos M et al (2012) Induction chemotherapy followed by concomitant radiotherapy and weekly cisplatin versus the same concomitant chemoradiotherapy in patients with nasopharyngeal carcinoma: a randomized phase II study conducted by the Hellenic Cooperative Oncology Group (HeCOG) with biomarker evaluation. Ann Oncol 23:427–435
Hong RL, Hsiao CF, Ting LL et al (2018) Final results of a randomized phase III trial of induction chemotherapy followed by concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in patients with stage IVA and IVB nasopharyngeal carcinoma-Taiwan Cooperative Oncology Group (TCOG) 1303 Study. Ann Oncol 29:1972–1979
Chen YP, Tang LL, Yang Q et al (2018) Induction chemotherapy plus concurrent chemoradiotherapy in endemic nasopharyngeal carcinoma: individual patient data pooled analysis of four randomized trials. Clin Cancer Res 24:1824–1833
Du X, Tang L, Chen L et al (2015) Neoadjuvant chemotherapy in locally advanced nasopharyngeal carcinoma: defining high-risk patients who may benefit before concurrent chemotherapy combined with intensity-modulated radiotherapy. Sci Rep 5:16664
Xu C, Sun R, Tang L et al (2018) Role of sequential chemoradiotherapy in stage II and low-risk stage III–IV nasopharyngeal carcinoma in the era of intensity-modulated radiotherapy: a propensity score-matched analysis. Oral Oncol 78:37–45
Zumsteg ZS, Luu M, Kim S et al (2018) Quantitative lymph node burden as a “very-high risk” factor identifying head and neck cancer patients benefiting from post-operative chemoradiation. Ann Oncol 30:76–84
Zhuo EH, Zhang WJ, Li HJ et al (2019) Radiomics on multi-modalities MR sequences can subtype patients with non-metastatic nasopharyngeal carcinoma (NPC) into distinct survival subgroups. Eur Radiol 29:5590–5599
Zhao L, Gong J, Xi Y et al (2019) MRI-based radiomics nomogram may predict the response to induction chemotherapy and survival in locally advanced nasopharyngeal carcinoma. Eur Radiol https://doi.org/10.1007/s00330-019-06211-x
Funding
This study was supported by Grant No. 61771007 from the National Natural Science Foundation of China; Grant No. 201907010043 from the Science and Technology Planning Project of Guangzhou City, China; Grant No. 703040078088 from the Science and Technology Development Special Funds (Frontier and Key Technology Innovation Direction – Major Science and Technology Project) of Guangdong Province; and Grant No. 201803010021 from the Health & Medical Collaborative Innovation Project of Guangzhou City.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Lizhi Liu.
Conflict of interest
The authors declare that they have conflict of interest.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the institutional review board.
Ethical approval
Institutional review board approval was obtained.
Methodology
• retrospective
• observational
• multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 211 kb)
Rights and permissions
About this article
Cite this article
Liu, Y., Chen, S., Dong, A. et al. Nodal grouping in nasopharyngeal carcinoma: prognostic significance, N classification, and a marker for the identification of candidates for induction chemotherapy. Eur Radiol 30, 2115–2124 (2020). https://doi.org/10.1007/s00330-019-06537-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06537-6