Abstract
Purpose
The goal of this study was to develop and evaluate a volumetric three-dimensional (3D) approach to improve the accuracy of ablation margin assessment following thermal ablation of hepatic tumors.
Methods
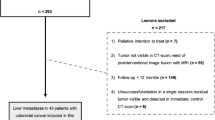
The 3D margin assessment technique was developed to generate the new 3D assessment metrics: volumes of insufficient coverage (VICs) measuring volume of tissue at risk post-ablation. VICs were computed for the tumor and tumor plus theoretical 5- and 10-mm margins. The diagnostic accuracy of the 3D assessment to predict 2-year local tumor progression (LTP) was compared to that of manual 2D assessment using retrospective analysis of a patient cohort that has previously been reported as a part of an outcome-centered study. Eighty-six consecutive patients with 108 colorectal cancer liver metastases treated with radiofrequency ablation (2002–2012) were used for evaluation. The 2-year LTP discrimination power was assessed using receiver operating characteristic area under the curve (AUC) analysis.
Results
A 3D assessment of margins was successfully completed for 93 out of 108 tumors. The minimum margin size measured using the 3D method had higher discrimination power compared with the 2D method, with an AUC value of 0.893 vs. 0.790 (p = 0.01). The new 5-mm VIC metric had the highest 2-year LTP discrimination power with an AUC value of 0.923 (p = 0.004).
Conclusions
Volumetric semi-automated 3D assessment of the ablation zone in the liver is feasible and can improve accuracy of 2-year LTP prediction following thermal ablation of hepatic tumors.
Key Points
• More accurate prediction of local tumor progression risk using volumetric 3D ablation zone assessment can help improve the efficacy of image-guided percutaneous thermal ablation of hepatic tumors.
• The accuracy of evaluation of ablation zone margins after thermal ablation of colorectal liver metastases can be improved using a volumetric 3D semi-automated assessment approach and the volume of insufficient coverage assessment metric.
• The new 5-mm volume-of-insufficient-coverage metric, indicating the volume of tumor plus 5-mm margin that remained untreated, had the highest 2-year local tumor progression discrimination power.



Similar content being viewed by others
Abbreviations
- LTP:
-
Local tumor progression
- 2D:
-
Two-dimensional
- 3D:
-
Three-dimensional
- AUC:
-
Area under the curve
- AZ:
-
Ablation zone
- CRLM:
-
Colorectal cancer liver metastases
- CT:
-
Computed tomography
- RFA:
-
Radiofrequency ablation
- VIC:
-
Volume of insufficient coverage
References
Gillams A, Lees W (2009) Five-year survival in 309 patients with colorectal liver metastases treated with radiofrequency ablation. Eur Radiol 19(5):1206–1213
Stang A, Fischbach R, Teichmann W, Bokemeyer C, Braumann D (2009) A systematic review on the clinical benefit and role of radiofrequency ablation as treatment of colorectal liver metastases. Eur J Cancer 45(10):1748–1756
Gillams A, Goldberg N, Ahmed M et al (2015) Thermal ablation of colorectal liver metastases: a position paper by an international panel of ablation experts, The Interventional Oncology Sans Frontières meeting 2013. Eur Radiol 25(12):3438–3454
Loveman E, Jones J, Clegg AJ et al (2014) The clinical effectiveness and cost-effectiveness of ablative therapies in the management of liver metastases: systematic review and economic evaluation. Health Technol Assess 18(7):1–283
van Amerongen MJ, Jenniskens SF, van den Boezem PB, Fütterer JJ, de Wilt JH (2017) Radiofrequency ablation compared to surgical resection for curative treatment of patients with colorectal liver metastases–a meta-analysis. HPB(Oxford) 19(9):749–756
Solbiati L, Ahmed M, Cova L, Ierace T, Brioschi M, Goldberg SN (2012) Small liver colorectal metastases treated with percutaneous radiofrequency ablation: local response rate and long-term survival with up to 10-year follow-up. Radiology 265(3):958–968
Hamada A, Yamakado K, Nakatsuka A et al (2012) Radiofrequency ablation for colorectal liver metastases: prognostic factors in non-surgical candidates. Jpn J Radiol 30(7):567–574
Napoleone M, Kielar AZ, Hibbert R, Saif S, Kwan BY (2016) Local tumor progression patterns after radiofrequency ablation of colorectal cancer liver metastases. Diagn Interv Radiol 22(6):548
Shady W, Petre EN, Gonen M et al (2015) Percutaneous radiofrequency ablation of colorectal cancer liver metastases: factors affecting outcomes—a 10-year experience at a single center. Radiology 278(2):601–611
Meijerink MR, Puijk RS, van Tilborg AAJM et al (2018) Radiofrequency and microwave ablation compared to systemic chemotherapy and to partial hepatectomy in the treatment of colorectal liver metastases: a systematic review and meta-analysis. Cardiovasc Intervent Radiol 41(8):1189–1204
Jeon SH, Cho YK, Choi SA, Kim MY, Lee HS (2017) Analysis of factors affecting local tumor progression of colorectal cancer liver metastasis after radiofrequency ablation. J Korean Soc Radiol 76(3):179–186
Shady W, Petre EN, Do KG et al (2017) Percutaneous microwave versus radiofrequency ablation of colorectal liver metastases: ablation with clear margins (A0) provides the best local tumor control. J Vasc Interv Radiol 29(2):268–275
Wang X, Sofocleous CT, Erinjeri JP et al (2013) Margin size is an independent predictor of local tumor progression after ablation of colon cancer liver metastases. Cardiovasc Intervent Radiol 36(1):166–175
Wakai T, Shirai Y, Sakata J et al (2008) Appraisal of 1 cm hepatectomy margins for intrahepatic micrometastases in patients with colorectal carcinoma liver metastasis. Ann Surg Oncol 15(9):2472–2481
Ahmed M, Solbiati L, Brace CL et al (2014) Image-guided tumor ablation: standardization of terminology and reporting criteria—a 10-year update. J Vasc Interv Radiol 25(11):1691–1705
Puijk RS, Ruarus AH, Scheffer HJ et al (2018) Percutaneous liver tumour ablation: image guidance, endpoint assessment, and quality control. Can Assoc Radiol J 69(1):51–62
Nakazawa T, Kokubu S, Shibuya A et al (2007) Radiofrequency ablation of hepatocellular carcinoma: correlation between local tumor progression after ablation and ablative margin. AJR Am J Roentgenol 188(2):480–488
Vogl TJ, Basten LM, Nour-Eldin N-EA et al (2017) Evaluation of microwave ablation of liver malignancy with enabled constant spatial energy control to achieve a predictable spherical ablation zone. Int J Hyperth 34(4):492–500
Goldberg SN, Grassi CJ, Cardella JF et al (2009) Image-guided tumor ablation: standardization of terminology and reporting criteria. J Vasc Interv Radiol 20(7):S377–SS90
Silverman SG, Sun MR, Tuncali K et al (2004) Three-dimensional assessment of MRI-guided percutaneous cryotherapy of liver metastases. AJR Am J Roentgenol 183(3):707–712
Passera K, Selvaggi S, Scaramuzza D, Garbagnati F, Vergnaghi D, Mainardi L (2013) Radiofrequency ablation of liver tumors: quantitative assessment of tumor coverage through CT image processing. BMC Med Imaging 13(1):3
Makino Y, Imai Y, Igura T et al (2015) Comparative evaluation of three-dimensional Gd-EOB-DTPA-enhanced MR fusion imaging with CT fusion imaging in the assessment of treatment effect of radiofrequency ablation of hepatocellular carcinoma. Abdom Imaging 40(1):102–111
Hocquelet A, Trillaud H, Frulio N et al (2016) Three-dimensional measurement of hepatocellular carcinoma ablation zones and margins for predicting local tumor progression. J Vasc Interv Radiol 27(7):1038–1045
Kim KW, Lee JM, Klotz E et al (2011) Safety margin assessment after radiofrequency ablation of the liver using registration of preprocedure and postprocedure CT images. AJR Am J Roentgenol 196(5):W565–WW72
Sakakibara M, Ohkawa K, Katayama K et al (2014) Three-dimensional registration of images obtained before and after radiofrequency ablation of hepatocellular carcinoma to assess treatment adequacy. AJR Am J Roentgenol 202(5):W487–WW95
Shin S, Lee JM, Kim KW et al (2014) Postablation assessment using follow-up registration of CT images before and after radiofrequency ablation (RFA): prospective evaluation of midterm therapeutic results of RFA for hepatocellular carcinoma. AJR Am J Roentgenol 203(1):70–77
Tani S, Tatli S, Hata N et al (2016) Three-dimensional quantitative assessment of ablation margins based on registration of pre-and post-procedural MRI and distance map. Int J Comput Assist Radiol Surg 11(6):1133–1142
Acknowledgements
We thank James Keller for his help with editing and preparing this manuscript.
Preliminary results were presented as an abstract during the RSNA 2017.
Funding
This research project was supported by an internal Department of Radiology seed grant and in part by the NIH/NCI Cancer Center Support Grant P30 CA008748.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Elena Kaye.
Conflict of interest
The authors of this manuscript declare relationships with the following companies.
C. T. Sofocleous has received research support from BTG, Ethicon (Neuwave); HS Medical, Angiodynamics; Sota Medical; and is a consultant for Ethicon and GE.
S. B. Solomon is a shareholder of Johnson & Johnson, Adgero, Immunomedics, Aspire Bariatrics, and Progenics; has received personal fees from Medtronics, BTG, Astra Zeneca, and Johnson & Johnson; and has a research grant from GE Heathcare.
J. Durack is an investor in and is on scientific advisory board of Adient Medical.
E. Kaye received consulting fees from Galil Medical.
The remaining authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Weiji Shi, PhD and Zhigang Zhang, PhD kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in:
1. Shady W, Petre EN, Gonen M, et al Percutaneous radiofrequency ablation of colorectal cancer liver metastases: factors affecting outcomes—a 10-year experience at a single center. Radiology. 2015;278:601–11.
2. Wang X, Sofocleous CT, Erinjeri JP, et al Margin size is an independent predictor of local tumor progression after ablation of colon cancer liver metastases. Cardiovasc Intervent Radiol 2013;36(1):166–175.
3. Sofocleous CT, Garg S, Petrovic LM, et al Ki-67 is a prognostic biomarker of survival after radiofrequency ablation of liver malignancies. Ann Surg Oncol 2012;19(13):4262–4269.
4. Sofocleous CT, Petre EN, Gonen M, et al CT-guided radiofrequency ablation as a salvage treatment of colorectal cancer hepatic metastases developing after hepatectomy. J Vasc Interv Radiol 2011;22(6):755–761.
Methodology
• Retrospective
• Diagnostic or prognostic study
• Performed at one institution
Electronic supplementary material
ESM 1
(DOCX 6556 kb)
Rights and permissions
About this article
Cite this article
Kaye, E.A., Cornelis, F.H., Petre, E.N. et al. Volumetric 3D assessment of ablation zones after thermal ablation of colorectal liver metastases to improve prediction of local tumor progression. Eur Radiol 29, 2698–2705 (2019). https://doi.org/10.1007/s00330-018-5809-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5809-0