Abstract
Objective
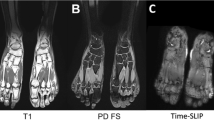
The purpose of this study is to develop a non-contrast magnetic resonance imaging (MRI) approach to evaluate skeletal muscle perfusion in the diabetic foot based on the concept of angiosomes of the foot.
Methods
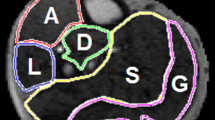
Five healthy volunteers and five participants with diabetes (HbA1c = 7.2 ± 1.8 %) without a history of peripheral artery disease were examined. The non-contrast perfusion measurements were performed during a toe flexion challenge. Absolute perfusion maps were created and two regions (medial and lateral) on the maps were segmented based on angiosomes.
Result
Regional difference in the perfusion of foot muscle was readily visualized in the MRI perfusion angiosomes during the challenge. In the participants with diabetes, the perfusion during toe flexion challenge was significantly lower than in healthy volunteers (P < 0.01). The average perfusion for the medial plantar region of the right foot was lower in subjects with diabetes (38 ± 9 ml/min/100 g) than in healthy subjects (93 ± 33 ml/min/100 g).
Conclusions
Non-contrast MRI perfusion angiosome maps demonstrate the feasibility of determining regional perfusion in foot muscles during toe challenge and may facilitate evaluation of muscle perfusion in diabetic feet.
Key Points
• Non-contrast MRI perfusion angiosome maps measure regional perfusion in foot muscles non-invasively.
• Foot perfusion response to challenge is reduced in persons with diabetes.
• MRI perfusion angiosome maps may help evaluation of regional foot muscle perfusion.




Similar content being viewed by others
References
Pecoraro RE, Reiber GE, Burgess EM (1990) Pathways to diabetic limb amputation. Basis for prevention. Diabetes Care 13:513–521
American Diabetes Association (1999) Consensus development conference on diabetic foot wound care: 7–8 April 1999, Boston, Massachusetts. Diabetes Care 22:1354–1360
Grunfeld C (1992) Diabetic foot ulcers: etiology, treatment and prevention. Adv Intern Med 37:103–132
Edmonds ME, Foster AVM (2000) Managing the diabetic foot. Blackwell Science Press, Oxford
Arora S, Pomposelli F, LoGerfo FW, Veves A (2002) Cutaneous microcirculation in the neuropathic diabetic foot improves significantly but not completely after successful lower extremity revascularization. J Vasc Surg 35:501–505
Apelqvist J, Elgzyri T, Larsson J, Löndahl M, Nyberg P, Thörne J (2011) Factors related to outcome of neuroischemic/ischemic foot ulcer in diabetic patients. J Vasc Surg 53:1582–1588
Cobb J, Claremont D (2002) Noninvasive measurement techniques for monitoring of microvascular function in the diabetic foot. Int J Low Extrem Wounds 1:161–169
Chao CYL, Cheing GLY (2009) Microvascular dysfunction in diabetic foot disease and ulceration. Diabetes Metab Res Rev 25:604–614
Taylor GI, Palmer JH (1987) The vascular territories (angiosomes) of the body: experimental studies and clinical applications. Br J Plast Surg 40:113–141
Alexandrescu V, Vincent G, Azdad K, Hubermont G, Ledent G, Ngongang C, Filimon AM (2011) A reliable approach to diabetic neuroischemic foot wounds: below-the-knee angiosome-oriented angioplasty. J Endovasc Ther 18:376–87
Zheng J, Hasting MK, Zhang X, Coggan A, An H, Snozek D, Curci J, Mueller MJ (2014) A pilot study of regional perfusion and oxygenation in calf muscles of diabetes with a noninvasive measure. J Vasc Surg 59:419–426
Zhang H, Shea SM, Park V, Li D, Woodard PK, Gropler RJ et al (2005) Accurate Myocardial T1 Measurements: Toward Quantification of Myocardial Blood Flow with Arterial Spin Labeling. Magn Reson Med 53:1135–1142
Zheng J, An H, Coggan AR, Zhang X, Bashir A, Muccigrosso D et al (2014) Non-contrast Skeletal Muscle Oximetry. Magn Reson Med 71:318–325
Fan Z, Sheehan J, Bi X, Liu X, Carr J, Li D (2009) 3D noncontrast MR angiography of the distal lower extremities using flow-sensitive dephasing (FSD)-prepared balanced SSFP. Magn Reson Med 62:1523–1532
Jung DY, Kim MH, Koh EK, Kwon OY, Cynn HS, Lee WH (2011) A comparison in the muscle activity of the abductor hallucis and the medial longitudinal arch angle during toe curl and short foot exercises. Phys Ther Sport 12:30–35
Hill T, Lewiki P (2006) Statistics methods and applications. StatSoft, Tulsa, pp 51–55
Lin CC, Ding HJ, Chen YW, Huang WT, Kao A (2004) Usefulness of thallium-201 muscle perfusion scan to investigate perfusion reserve in the lower limbs of Type 2 diabetic patients. J Diabet Complicat 18:233–236
Springer F, Steidle G, Martirosian P, Syha R, Claussen CD, Schick F (2011) Rapid assessment of longitudinal relaxation time in materials and tissues with extremely fast signal decay using UTE sequences and the variable flip angle method. Invest Radiol 46:610–617
Filho GH, Du J, Pak BC, Statum S, Znamorowski R, Haghighi P, Bydder G, Chung CB (2009) Quantitative characterization of the Achilles tendon in cadaveric specimens: T1 and T2* measurements using ultrashort-TE MRI at 3 T. AJR Am J Roentgenol 192:W117–124
Spriet M, Wisner ER, Anthenill LA, Buonocore MH (2011) Determination of T1 relaxation time of normal equine tendons using magic angle magnetic resonance imaging. Vet Radiol Ultrasound 52:149–153
Cheuy VA, Hastings MK, Commean PK, Ward SR, Mueller MJ (2013) Intrinsic foot muscle deterioration is associated with metatarsophalangeal joint angle in people with diabetes and neuropathy. Clin Biomech 28:1055–60
Brash PD, Foster J, Vennart W, Anthony P, Tooke JE (1999) Magnetic resonance imaging techniques demonstrate soft tissue damage in the diabetic foot. Diabet Med 16:55–61
Suzuki E, Kashiwagi A, Hidaka H, Maegawa H, Nishio Y, Kojima H, Haneda M, Yasuda H, Morikawa S, Inubushi T, Kikkawa R (2000) 1H- and 31P-magnetic resonance spectroscopy and imaging as a new diagnostic tool to evaluate neuropathic foot ulcers in type II diabetic patients. Diabetologia 43:165–172
Bus SA, Maas M, Lindeboom R (2006) Reproducibility of foot structure measurements in neuropathic diabetic patients using magnetic resonance imaging. J Magn Reson Imaging 24:25–32
Huang Y, Majumdar S, Genant HK, Chan WP, Sharma KR, Yu P, Mynhier M, Miller RG (1994) Quantitative MR relaxometry study of muscle composition and function in Duchenne muscular dystrophy. J Magn Reson Imaging 4:59–64
Lim RP, Fan Z, Chatterji M, Baadh A, Atanasova IP, Storey P, Kim DC, Kim S, Hodnett PA, Ahmad A, Stoffel DR, Babb JS, Adelman MA, Xu J, Li D, Lee VS (2013) Comparison of nonenhanced MR angiographic subtraction techniques for infragenual arteries at 1.5 T: a preliminary study. Radiology 267:293–304
Zimny S, Dessel F, Ehren M, Pfohl M, Schatz H (2001) Early detection of microcirculatory impairment in diabetic patients with foot at risk. Diabetes Care 24:1810–1814
Hile C, Veves A (2003) Diabetic neuropathy and microcirculation. Curr Diab Rep 3:446–451
Baker N, Green A, Krishnan S, Rayman G (2007) Microvascular and C-fiber function in diabetic charcot neuroarthropathy and diabetic peripheral neuropathy. Diabetes Care 30:3077–3079
Sun PC, Kuo CD, Chi LY, Lin HD, Wei SH, Chen CS (2013) Microcirculatory vasomotor changes are associated with severity of peripheral neuropathy in patients with type 2 diabetes. Diab Vasc Dis Res 10:270–276
Tomešová J, Gruberova J, Lacigova S, Cechurova D, Jankovec Z, Rusavy Z (2013) Differences in skin microcirculation on the upper and lower extremities in patients with diabetes mellitus: relationship of diabetic neuropathy and skin microcirculation. Diabetes Technol Ther 15:968–975
Acknowledgments
Research reported in this publication was supported partially by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH), a research grant from Diabetes Action Research and Education Foundation, and the Mallinckrodt Institute of Radiology. The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH. The authors thank Darrah Snozek for assistance in subject recruitment.
The scientific guarantor of this publication is Jie Zheng. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. No complex statistical methods were necessary for this paper. Washington University in St. Louis Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Methodology: prospective, experimental, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zheng, J., Hastings, M.K., Muccigross, D. et al. Non-contrast MRI perfusion angiosome in diabetic feet. Eur Radiol 25, 99–105 (2015). https://doi.org/10.1007/s00330-014-3337-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3337-0