Abstract
Purpose
Blood-derived proliferative factors such as platelet rich plasma or activated plasma are promising adjuvants for bone grafts. Our earlier studies showed that serum albumin itself can markedly enhance the proliferation of stem cells on bone allograft and postulated that albumin coating alone may improve bone graft integration in vivo.
Methods
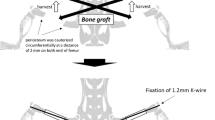
Two femoral defect models were performed in adult male Wistar rats. In the critical size model a six millimetre gap was created in the midshaft of the femur and fixed with plate and screws, while a nonunion model was established by the interposition of a spacer in the osteotomy for four weeks which resulted in compromised healing and nonunion. Albumin coated and uncoated grafts were placed into the defects. Bone healing and morphometry were evaluated by μCT and histology four weeks after implantation of the grafts.
Results
In the critical size model none of the bone grafts were able to bridge the defect, and graft resorption was the typical outcome. In the nonunion model regular uncoated grafts had a low union rate (two out of six), which increased markedly when albumin coating was applied (six out of eight). Trabecular thickness and pattern factor improved significantly in the albumin coated group versus uncoated or empty controls.
Conclusions
Our results showed that serum albumin coating of bone grafts can enhance the remodelling and efficacy of treatment in a nonunion model.




Similar content being viewed by others
References
Bae JH, Kim YK, Myung SK (2011) Effects of platelet-rich plasma on sinus bone graft: meta-analysis. J Periodontol 82:660–667
Bae HW, Zhao L, Kanim LEA, Wong P, Delamarter RB, Dawson EG (2006) Intervariability and intravariability of bone morphogenetic proteins in commercially available demineralized bone matrix products. Spine 31:1299–1306
Bishop GB, Einhorn TA (2007) Current and future clinical applications of bone morphogenetic proteins in orthopaedic trauma surgery. Int Orthop 31:721–727
Cooper GM, Mooney MP, Gosain AK, Campbell PG, Losee JE, Huard J (2010) Testing the critical size in calvarial bone defects: revisiting the concept of a critical-size defect. Plast Reconstr Surg 125:1685–1692
Dimitriou R, Mataliotakis GI, Angoules AG, Kanakaris NK, Giannoudis PV (2011) Complications following autologous bone graft harvesting from the iliac crest and using the RIA: a systematic review. Injury 42(Suppl 2):S3–S15
Gamradt SC, Lieberman JR (2003) Bone graft for revision hip arthroplasty: biology and future applications. Clin Orthop Relat Res 417:183–194
Gosain AK, Song L, Yu P (2000) Osteogenesis in cranial defects: reassessment of the concept of critical size and the expression of TGF-beta isoforms. Plast Reconstr Surg 106:360–372
Hao W, Dong J, Jiang M, Wu J, Cui F, Zhou D (2010) Enhanced bone formation in large segmental radial defects by combining adipose-derived stem cells expressing bone morphogenetic protein 2 with nHA/RHLC/PLA scaffold. Int Orthop 34:1341–1349
Jiang ZQ, Liu HY, Zhang LP, Wu ZQ, Shang DZ (2012) Repair of calvarial defects in rabbits with platelet-rich plasma as the scaffold for carrying bone marrow stromal cells. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 113:327–333
Johannes C, Reichert JC, Saifzadeh S, Wullschleger ME, Epari DR, Schütz MA, Duda GN, Schell H, Van Griensven M, Redl H, Hutmacher DW (2009) The challenge of establishing preclinical models for segmental bone defect research. Biomaterials 30:2149–2163
Kanthan SR, Kavitha G, Addi S, Choon DS, Kamarul T (2011) Platelet-rich plasma (PRP) enhances bone healing in non-united critical-sized defects: a preliminary study involving rabbit models. Injury 42:782–789
Lindsey RW, Gugala Z, Milne E, Sun M, Gannon FH, Latta LL (2006) The efficacy of cylindrical titanium mesh cage for the reconstruction of a critical-size canine segmental femoral diaphyseal defect. J Orthop Res 24:1438–1453
Muschler GF, Lane JM, Werntz J, Gebhardt M, Sandu H, Piergentili C, Nottebaert M, Baker C, Burstein A (1989) Segmental femoral defect model in the rat. In: Aebi M, Regazzoni P (eds) Bone transplantation. Springer, New York, pp 167–169
Oakes DA, Lee C, Lieberman JR (2003) An evaluation of human demineralized bone matrices in a rat femoral defect model. Clin Orthop 413:281–290
Pape HC, Evans A, Kobbe PJ (2010) Autologous bone graft: properties and techniques. Orthop Trauma 24(Suppl 1):S36–S40
Pecina M, Haspl M, Jelic M, Vukicevic S (2003) Repair of a resistant tibia non-union with a recombinant bone morphogenetic protein-7 (rh-BMP-7). Int Orthop 27:320–321
Peerbooms JC, Colaris JW, Hakkert AA, Van Appeldorn M, Bruijn DJ, Den Oudsten BL, Gosens T (2012) No positive bone healing after using platelet rich plasma in a skeletal defect. An observational prospective cohort study. Int Orthop 36:2113–2119
Rimondini L, Nicoli-Aldini N, Fini M, Guzzardella G, Tschon M, Giardino R (2005) In vivo experimental study on bone regeneration in critical bone defects using an injectable biodegradable PLA/PGA copolymer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 99:148–154
Schmidhammer R, Zandieh S, Mittermayr R, Pelinka LE, Leixnering M, Hopf R, Kroepfl A, Redl H (2006) Assessment of bone union/nonunion in an experimental model using microcomputed technology. J Trauma 61:199–205
Skaliczki G, Weszl M, Schandl K, Major T, Kovács M, Skaliczki J, Redl H, Szendrői M, Szigeti K, Máté D, Dobó-Nagy C, Lacza Z (2012) Compromised bone healing following spacer removal in a rat femoral defect model. Acta Physiol Hung 99:223–232
Southerland D, Bostrom M (2005) Grafts and bone graft substitutes. In: Lieberman JR, Friedlaender GE (eds) Bone regeneration and repair. Humana Press, Totowa, NJ, pp 133–56
Verna C, Dalstra M, Wikesjo UM, Trombelli L (2002) Healing patterns in calvarial bone defects following guided bone regeneration in rats. A micro-CT scan analysis. J Clin Periodontol 29:865–870
Weszl M, Skaliczki G, Cselenyák A, Kiss L, Major T, Schandl K, Bognár E, Stadler G, Peterbauer A, Csönge L, Lacza Z (2012) Freeze-dried human serum albumin improves the adherence and proliferation of mesenchymal stem cells on mineralized human bone allografts. J Orthop Res 30:489–496
Urist MR (1965) Bone: formation by autoinduction. Science 150:893–899
Yilmaz S, Kabadayi C, Ipci SD, Cakar G, Kuru B (2011) Treatment of intrabony periodontal defects with platelet-rich plasma versus platelet-poor plasma combined with a bovine-derived xenograft: a controlled clinical trial. J Periodontol 82:837–844
Acknowledgments
We are thankful for Lacerta Technologies Inc. and the West-Hungarian Tissue Bank for providing the bone grafts. The present work was funded by grants from TÉT-SIN-CELLTHER, TÁMOP-4.2.1/B09/1/KMR-2010-0001, OTKA 83803.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Skaliczki, G., Schandl, K., Weszl, M. et al. Serum albumin enhances bone healing in a nonunion femoral defect model in rats: a computer tomography micromorphometry study. International Orthopaedics (SICOT) 37, 741–745 (2013). https://doi.org/10.1007/s00264-012-1770-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-012-1770-8