Abstract
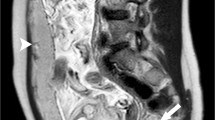
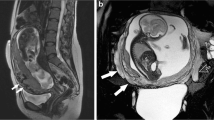
Appropriate placentation is critical to maternal and fetal outcomes. Abnormal placentation, including placenta previa and morbidly adherent placenta, is increasing in incidence and is associated with multiple risk factors including advanced maternal age and history of prior cesarean delivery. Magnetic resonance imaging (MRI) is increasingly used in assessing the type and extent of abnormal placentation, often leading to modifications in surgical approach. Here, we review the MRI features and appropriate reporting of placenta previa and the placenta accreta spectrum.











Similar content being viewed by others
References
Committee on Obstetric Practice (2012) Committee Opinion No. 529: placenta accreta. Obstet Gynecol 120:207–211
Masselli G, Brunelli R, Casciani E, et al. (2008) Magnetic resonance imaging in the evaluation of placental adhesive disorders: correlation with color Doppler ultrasound. Eur Radiol 18:1292–1299
Lim PS, Greenberg M, Edelson MI, et al. (2011) Utility of ultrasound and MRI in prenatal diagnosis of placenta accreta: a pilot study. AJR Am J Roentgenol 197:1506–1513
Palacios Jaraquemada JM, Bruno CH (2005) Magnetic resonance imaging in 300 cases of placenta accreta: surgical correlation of new findings. Acta Obstet Gynecol Scand 84:716–724
Levine D, Hulka CA, Ludmir J, Li W, Edelman RR (1997) Placenta accreta: evaluation with color Doppler US, power Doppler US, and MR imaging. Radiology 205:773–776
Lax A, Prince MR, Mennitt KW, Schwebach JR, Budorick NE (2007) The value of specific MRI features in the evaluation of suspected placental invasion. Magn Reson Imaging 25:87–93
Victoria T, Jaramillo D, Roberts TPL, et al. (2014) Fetal magnetic resonance imaging: jumping from 1.5 to 3 tesla (preliminary experience). Pediatr Radiol 44:376–386 (quiz 373–375)
Merkle EM, Dale BM, Paulson EK (2006) Abdominal MR imaging at 3T. Magn Reson Imaging Clin N Am 14:17–26
Derman AY, Nikac V, Haberman S, et al. (2011) MRI of placenta accreta: a new imaging perspective. AJR Am J Roentgenol 197:1514–1521
Masselli G, Brunelli R, Parasassi T, Perrone G, Gualdi G (2011) Magnetic resonance imaging of clinically stable late pregnancy bleeding: beyond ultrasound. Eur Radiol 21:1841–1849
Siauve N, Chalouhi GE, Deloison B, et al. (2015) Functional imaging of the human placenta with magnetic resonance. Am J Obstet Gynecol 213:S103–S114
Kanal E, Barkovich AJ, Bell C, et al. (2007) ACR guidance document for safe MR practices: 2007. AJR Am J Roentgenol 188:1447–1474
Kanda T, Fukusato T, Matsuda M, et al. (2015) Gadolinium-based contrast agent accumulates in the brain even in subjects without severe renal dysfunction: evaluation of autopsy brain specimens with inductively coupled plasma mass spectroscopy. Radiology 276:228–232
Kanda T, Osawa M, Oba H, et al. (2015) High signal intensity in dentate nucleus on unenhanced T1-weighted MR images: association with linear versus macrocyclic gadolinium chelate administration. Radiology 275:803–809
McDonald RJ, McDonald JS, Kallmes DF, et al. (2015) Intracranial gadolinium deposition after contrast-enhanced MR imaging. Radiology 275:772–782
Errante Y, Cirimele V, Mallio CA, et al. (2014) Progressive increase of T1 signal intensity of the dentate nucleus on unenhanced magnetic resonance images is associated with cumulative doses of intravenously administered gadodiamide in patients with normal renal function, suggesting dechelation. Invest Radiol 49:685–690
Okuda Y, Sagami F, Tirone P, et al. (1999) Reproductive and developmental toxicity study of gadobenate dimeglumine formulation (E7155) (3)—study of embryo-fetal toxicity in rabbits by intravenous administration. J Toxicol Sci 24(Suppl 1):79–87
Tanaka YO, Sohda S, Shigemitsu S, Niitsu M, Itai Y (2001) High temporal resolution dynamic contrast MRI in a high risk group for placenta accreta. Magn Reson Imaging 19:635–642
Riteau A-S, Tassin M, Chambon G, et al. (2014) Accuracy of ultrasonography and magnetic resonance imaging in the diagnosis of placenta accreta. PLoS ONE 9:e94866
Brosens JJ, Pijnenborg R, Brosens IA (2002) The myometrial junctional zone spiral arteries in normal and abnormal pregnancies: a review of the literature. Am J Obstet Gynecol 187:1416–1423
Baergen Rebecca N (2005) Manual of Benirschke and Kaufmann’s pathology of the human placenta. New York: Springer
Clark SL, Koonings PP, Phelan JP (1985) Placenta previa/accreta and prior cesarean section. Obstet Gynecol 66:89–92
Nielsen TF, Hagberg H, Ljungblad U (1989) Placenta previa and antepartum hemorrhage after previous cesarean section. Gynecol Obstet Invest 27:88–90
Rao KP, Belogolovkin V, Yankowitz J, Spinnato JA (2012) Abnormal placentation: evidence-based diagnosis and management of placenta previa, placenta accreta, and vasa previa. Obstet Gynecol Surv 67:503–519
Miller DA, Chollet JA, Goodwin TM (1997) Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol 177:210–214
Reddy UM, Abuhamad AZ, Levine D, Saade GR (2014) Fetal imaging: executive summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecolog. J Ultrasound Med 33:745–757
Wexler P, Gottesfeld KR (1979) Early diagnosis of placenta previa. Obstet Gynecol 54:231–234
Heller HT, Mullen KM, Gordon RW, Reiss RE, Benson CB (2014) Outcomes of pregnancies with a low-lying placenta diagnosed on second-trimester sonography. J Ultrasound Med 33:691–696
Wu S, Kocherginsky M, Hibbard JU (2005) Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol 192:1458–1461
Hung TH, Shau WY, Hsieh CC, et al. (1999) Risk factors for placenta accreta. Obstet Gynecol 93:545–550
Bour L, Placé V, Bendavid S, et al. (2014) Suspected invasive placenta: evaluation with magnetic resonance imaging. Eur Radiol 24:3150–3160
Silver RM, Landon MB, Rouse DJ, et al. (2006) Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol 107:1226–1232
Ueno Y, Kitajima K, Kawakami F, et al. (2014) Novel MRI finding for diagnosis of invasive placenta praevia: evaluation of findings for 65 patients using clinical and histopathological correlations. Eur Radiol 24:881–888
Gielchinsky Y, Rojansky N, Fasouliotis SJ, Ezra Y (2002) Placenta accreta—summary of 10 years: a survey of 310 cases. Placenta 23:210–214
Usta IM, Hobeika EM, Musa AAA, Gabriel GE, Nassar AH (2005) Placenta previa-accreta: risk factors and complications. Am J Obstet Gynecol 193:1045–1049
Timor-Tritsch IE, Monteagudo A, Cali G, et al. (2014) Cesarean scar pregnancy and early placenta accreta share common histology. Ultrasound Obstet Gynecol 43:383–395
Timor-Tritsch IE, Monteagudo A, Cali G, et al. (2014) Cesarean scar pregnancy is a precursor of morbidly adherent placenta. Ultrasound Obstet Gynecol 44:346–353
Zelop C, Nadel A, Frigoletto FD, et al. (1992) Placenta accreta/percreta/increta: a cause of elevated maternal serum alpha-fetoprotein. Obstet Gynecol 80:693–694
Leyendecker JR, DuBose M, Hosseinzadeh K, et al. (2012) MRI of pregnancy-related issues: abnormal placentation. AJR Am J Roentgenol 198:311–320
Bretelle F, Courbière B, Mazouni C, et al. (2007) Management of placenta accreta: morbidity and outcome. Eur J Obstet Gynecol Reprod Biol 133:34–39
Hudon L, Belfort MA, Broome DR (1998) Diagnosis and management of placenta percreta: a review. Obstet Gynecol Surv 53:509–517
Meng X, Xie L, Song W (2013) Comparing the diagnostic value of ultrasound and magnetic resonance imaging for placenta accreta: a systematic review and meta-analysis. Ultrasound Med Biol 39:1958–1965
D’Antonio F, Iacovella C, Palacios-Jaraquemada J, et al. (2014) Prenatal identification of invasive placentation using magnetic resonance imaging: systematic review and meta-analysis. Ultrasound Obstet Gynecol 44:8–16
American College of Obstetricians and Gynecologists. (2009) ACOG Practice Bulletin No. 101: ultrasonography in pregnancy. Obstet Gynecol 113:451–461
Horowitz JM, Berggruen S, McCarthy RJ, et al. (2015) When timing is everything: are placental MRI examinations performed before 24 weeks’ gestational age reliable? AJR Am J Roentgenol 205:685–692
Warshak CR, Eskander R, Hull AD, et al. (2006) Accuracy of ultrasonography and magnetic resonance imaging in the diagnosis of placenta accreta. Obstet Gynecol 108:573–581
Dwyer BK, Belogolovkin V, Tran L, et al. (2008) Prenatal diagnosis of placenta accreta: sonography or magnetic resonance imaging? J Ultrasound Med 27:1275–1281
Elhawary TM, Dabees NL, Youssef MA (2013) Diagnostic value of ultrasonography and magnetic resonance imaging in pregnant women at risk for placenta accreta. J Matern Fetal Neonatal Med 26:1443–1449
Rahaim NSA, Whitby EH (2015) The MRI features of placental adhesion disorder and their diagnostic significance: systematic review. Clin Radiol 70:917–925
Alamo L, Anaye A, Rey J, et al. (2013) Detection of suspected placental invasion by MRI: do the results depend on observer’ experience? Eur J Radiol 82:e51–e57
Kim JA, Narra VR (2004) Magnetic resonance imaging with true fast imaging with steady-state precession and half-Fourier acquisition single-shot turbo spin-echo sequences in cases of suspected placenta accreta. Acta Radiol 45:692–698
Teo TH, Law YM, Tay KH, Tan BS, Cheah FK (2009) Use of magnetic resonance imaging in evaluation of placental invasion. Clin Radiol 64:511–516
Noda Y, Kanematsu M, Goshima S, et al. (2015) Prenatal MR imaging diagnosis of placental invasion. Abdom Imaging 40:1273–1278
Blaicher W, Brugger PC, Mittermayer C, et al. (2006) Magnetic resonance imaging of the normal placenta. Eur J Radiol 57:256–260
Baughman WC, Corteville JE, Shah RR. Placenta accreta: spectrum of US and MR imaging findings. Radiographics. 28:1905–1916.
Elchalal U, Ezra Y, Levi Y, et al. (2000) Sonographically thick placenta: a marker for increased perinatal risk—a prospective cross-sectional study. Placenta 21:268–272
Hoddick WK, Mahony BS, Callen PW, Filly RA (1985) Placental thickness. J Ultrasound Med 4:479–482
Lee AJ, Bethune M, Hiscock RJ (2012) Placental thickness in the second trimester: a pilot study to determine the normal range. J Ultrasound Med 31:213–218
Akgündüz E, Erkılınç S, Tokmak A, et al. (2015) Decreased placental thickness and impaired Doppler indices in idiopathic polyhydramnios: a prospective case-control study. J Matern Fetal Neonatal Med 28:722–725
Funding
This study did not receive funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Lea Azour declares that she has no conflict of interest. Cecilia Besa declares that she has no conflict of interest. Sara Lewis declares that she has no conflict of interest. Amita Kamath declares that she has no conflict of interest. Edward R. Olive declares that he has no conflict of interest. Bachir Taouli declares that he has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Azour, L., Besa, C., Lewis, S. et al. The gravid uterus: MR imaging and reporting of abnormal placentation. Abdom Radiol 41, 2411–2423 (2016). https://doi.org/10.1007/s00261-016-0752-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0752-5