Abstract
Introduction
The decision on thrombolytics administration is usually based on a generalized, rigid time-based rule rather than an individualized evaluation of the “tissue at risk of infarction” which is the target of the recanalization therapies. The goals of our article are to assess whether there is tissue at risk of infarction in a group of acute stroke patients treated beyond 8 h after symptom onset and to investigate the baseline imaging and clinical features that predict the fate of this tissue at risk.
Methods
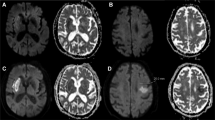
We retrospectively reviewed a series of patients with acute ischemic stroke treated with endovascular recanalization therapies beyond 8 h after symptom onset. The tissue at risk was calculated as the difference between the infarct volumes on baseline and follow-up imaging (infarct growth). We analyzed the epidemiological distribution of infarct growth, and we performed a multivariate regression analysis to identify the baseline variables that predict infarct growth.
Results
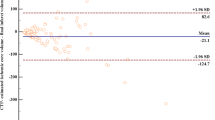
Our study group included 75 patients (65 ± 13.8 years, baseline National Institutes of Health Stroke Scale 14 ± 4.9, time to treatment 15.2 ± 8.7 h). The mean infarct growth was 78.6 ± 95.0 cc (p < 0.001), and, overall, the infarct growth was greater when the baseline volume of infarct tissue was small (p < 0.001) and in the case of a unsuccessful arterial recanalization (p = 0.001).
Conclusions
There is potentially salvageable ischemic tissue at risk in acute stroke patients treated beyond 8 h after symptom onset.


Similar content being viewed by others
References
Bambauer KZ, Johnston SC, Bambauer DE, Zivin JA (2006) Reasons why few patients with acute stroke receive tissue plasminogen activator. Arch Neurol 63:661–664
Hacke W, Kaste M, Bluhmki E et al (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 359:1317–1329
Copen WA, Rezai Gharai L, Barak ER et al (2009) Existence of the diffusion-perfusion mismatch within 24 hours after onset of acute stroke: dependence on proximal arterial occlusion. Radiology 250:878–886
Read SJ, Hirano T, Abbott DF et al (2000) The fate of hypoxic tissue on 18F-fluoromisonidazole positron emission tomography after ischemic stroke. Ann Neurol 48:228–235
Read SJ, Hirano T, Abbott DF et al (1998) Identifying hypoxic tissue after acute ischemic stroke using PET and 18F-fluoromisonidazole. Neurology 51:1617–1621
Albers GW, Thijs VN, Wechsler L et al (2006) Magnetic resonance imaging profiles predict clinical response to early reperfusion: the diffusion and perfusion imaging evaluation for understanding stroke evolution (DEFUSE) study. Ann Neurol 60:508–517
Furlan AJ, Eyding D, Albers GW et al (2006) Dose escalation of desmoteplase for acute ischemic stroke (DEDAS): evidence of safety and efficacy 3 to 9 hours after stroke onset. Stroke 37:1227–1231
Hacke W, Albers G, Al-Rawi Y et al (2005) The desmoteplase in acute ischemic stroke trial (DIAS): a phase II MRI-based 9-hour window acute stroke thrombolysis trial with intravenous desmoteplase. Stroke 36:66–73
Lees KR, Bluhmki E, von Kummer R et al (2010) Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet 375:1695–1703
Saver JL, Levine SR (2010) Alteplase for ischaemic stroke—much sooner is much better. Lancet 375:1667–1668
Khatri P, Abruzzo T, Yeatts SD et al (2009) Good clinical outcome after ischemic stroke with successful revascularization is time-dependent. Neurology 73:1066–1072
Zangerle A, Kiechl S, Spiegel M et al (2007) Recanalization after thrombolysis in stroke patients: predictors and prognostic implications. Neurology 68:39–44
Kidwell CS, Alger JR, Saver JL (2003) Beyond mismatch: evolving paradigms in imaging the ischemic penumbra with multimodal magnetic resonance imaging. Stroke 34:2729–2735
Abou-Chebl A (2010) Endovascular treatment of acute ischemic stroke may be safely performed with no time window limit in appropriately selected patients. Stroke 41:1996–2000
Jovin TG, Liebeskind DS, Gupta R et al (2011) Imaging-based endovascular therapy for acute ischemic stroke due to proximal intracranial anterior circulation occlusion treated beyond 8 hours from time last seen well: retrospective multicenter analysis of 237 consecutive patients. Stroke 42:2206–2211
Furlan A, Higashida R, Wechsler L et al (1999) Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA 282:2003–2011
Jovin TG, Yonas H, Gebel JM et al (2003) The cortical ischemic core and not the consistently present penumbra is a determinant of clinical outcome in acute middle cerebral artery occlusion. Stroke 34:2426–2433
Rha JH, Saver JL (2007) The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke 38:967–973
Poisson SN, Nguyen-Huynh MN, Johnston SC, Furie KL, Lev MH, Smith WS (2011) Intracranial large vessel occlusion as a predictor of decline in functional status after transient ischemic attack. Stroke 42:44–47
Smith WS, Lev MH, English JD et al (2009) Significance of large vessel intracranial occlusion causing acute ischemic stroke and TIA. Stroke 40:3834–3840
Rosso C, Colliot O, Valabrègue R et al (2011) Tissue at risk in the deep middle cerebral artery territory is critical to stroke outcome. Neuroradiology 53:763–71
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
ESM 1
(DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Leiva-Salinas, C., Aghaebrahim, A., Zhu, G. et al. Tissue at risk in acute stroke patients treated beyond 8 h after symptom onset. Neuroradiology 55, 807–812 (2013). https://doi.org/10.1007/s00234-013-1164-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-013-1164-7