Abstract
Rationale
Despite decades of research, tardive dyskinesia (TD) remains a poorly understood iatrogenic movement disorder with few effective treatments and no known cure. Accordingly, the development of an innocuous strategy to prevent or mitigate antipsychotic (AP)-associated TD would represent an important clinical advance. Supporting evidence for antioxidant (AX)-based treatment regimens can be found in the preclinical literature, where AP-induced vacuous chewing movements (VCMs) in rats are attenuated by the concurrent administration of direct and indirect AXs.
Objectives
Our aim was to review the preclinical literature examining the role of AX-promoting treatments in the prevention of AP-induced VCMs in rats.
Methods
A literature search using Google Scholar and PubMed was performed. Relevant results were qualitatively reviewed.
Results
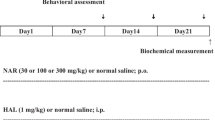
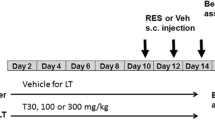
Studies featuring a variety of naturally occurring and synthetic AX treatments were identified and included in the review. The majority of studies used haloperidol (HAL), a typical AP, to induce VCMs. Studies revealed reduced VCMs in co-treated rats, with favorable changes seen in markers of oxidative stress (OS) and AX status, but were limited by their short durations.
Conclusions
Some preclinical evidence suggests that the inclusion of a naturally occurring and benign AX compound as an adjunct to AP treatment may help guard patients against TD, but additional long-duration studies are needed. This AX-based strategy is further substantiated by accumulating evidence of preexisting OS abnormalities in schizophrenia (SZ).

Similar content being viewed by others
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders- 5. APA Press, Arlington
Andreassen OA, Jørgensen HA (2000) Neurotoxicity associated with neuroleptic-induced oral dyskinesias in rats: implications for tardive dyskinesia? Prog Neurobiol 61:525–541
Andreassen OA, Weber C, Jørgensen HA (1999) Coenzyme Q10 does not prevent oral dyskinesias induced by long-term haloperidol treatment of rats. Pharmacol Biochem Behav 64:637–642
Barcelos RCS, Benvegnú DM, Boufleur N, Reckziegel P, Müller LG, Pase C, Emanuelli T, Bürger ME (2010) Effects of ω-3 essential fatty acids (ω-3 EFAs) on motor disorders and memory dysfunction typical neuroleptic-induced: behavioral and biochemical parameter. Neurotox Res 17:228–237
Bentinger M, Dallner G, Chojnacki T, Swiezewska E (2003) Distribution and breakdown of labeled coenzyme Q10 in rat. Free Radical Bio Med 34:563–575
Benvegnú DM, Barcelos RCS, Boufleur N, Pase CS, Reckziegel P, Flores FC, Ourique AF, Nora MD, da Silva CDB, Beck RCR, Bürger ME (2012) Haloperidol-loaded polysorbate-coated polymeric nanocapsules decrease its adverse motor side effects and oxidative stress markers in rats. Neurochem Int 61:623–631
Betti M, Minelli A, Ambrogini P, Ciuffoli S, Viola V, Galli F, Canonico B, Lattanzi D, Colombo E, Sestili P, Cuppini R (2011) Dietary supplementation with α-tocopherol reduces neuroinflammation and neuronal degeneration in the rat brain after kainic acid-induced status epilepticus. Free Radical Res 45:1136–1142
Bezchlibnyk-Butler KZ, Jeffries JJ (2005) Clinical handbook of psychotropic drugs. Hogrefe and Huber Publishers, Toronto
Bhidayasiri R, Fahn S, Weiner WJ, Gronseth GS, Sullivan KL, Zesiewicz TA (2013) Evidence-based guideline: treatment of tardive syndromes. Neurology 81:463–469
Bishnoi M, Chopra K, Kulkarni SK (2006) Involvement of adenosinergic receptor system in an animal model of tardive dyskinesia and associated behavioural, biochemical and neurochemical changes. Eur J Pharmacol 552:55–66
Bishnoi M, Chopra K, Kulkarni SK (2007a) U-74500A (Lazaroid), a 21-aminosteroid attenuates neuroleptic-induced orofacial dyskinesia. Method Find Exp Clin 29:601–605
Bishnoi M, Chopra K, Kulkarni SK (2007b) Possible anti-oxidant and neuroprotective mechanisms of zolpidem in attenuating typical anti-psychotic-induced orofacial dyskinesia—a biochemical and neurochemical study. Prog Neuro-Psychoph 31:1130–1138
Bishnoi M, Chopra K, Kulkarni SK (2007c) Protective effect of rutin, a polyphenolic flavonoid against haloperidol-induced orofacial dyskinesia and associated behavioural, biochemical and neurochemical changes. Fund Clin Pharmacol 21:521–529
Bishnoi M, Chopra K, Kulkarni SK (2007d) Theophylline, adenosine receptor antagonist prevents behavioral, biochemical and neurochemical changes associated with an animal model of tardive dyskinesia. Pharmacol Rep 59:181–191
Bishnoi M, Chopra K, Kulkarni SK (2007e) Protective effect of adenosine reuptake inhibitors in haloperidol-induced orofacial dyskinesia and associated behavioural, biochemical and neurochemical changes. Pharmacology 79:171–183
Bishnoi M, Chopra K, Kulkarni SK (2008a) Modulatory effect of neurosteroids in haloperidol-induced vacuous chewing movements and related behaviors. Psychopharmacology 196:243–254
Bishnoi M, Chopra K, Kulkarni SK (2008b) Protective effect of curcumin, the active principle of turmeric (Curcuma longa) in haloperidol-induced orofacial dyskinesia and associated behavioural, biochemical and neurochemical changes in rat brain. Pharmacol Biochem Behav 88:511–522
Bishnoi M, Chopra K, Kulkarni SK (2008c) Progesterone attenuates neuroleptic-induced orofacial dyskinesia via the activity of its metabolite, allopregnanolone, a positive GABAA modulating neurosteroid. Prog Neuro-Psychoph 32:451–461
Bishnoi M, Chopra K, Kulkarni SK (2008d) Protective effect of L-type calcium channel blockers against haloperidol-induced orofacial dyskinesia: a behavioural, biochemical and neurochemical study. Neurochem Res 33:1869–1880
Bishnoi M, Chopra K, Kulkarni SK (2009) Co-administration of nitric oxide (NO) donors prevents haloperidol-induced orofacial dyskinesia, oxidative damage and change in striatal dopamine levels. Pharmacol Biochem Behav 91:423–429
Bishnoi M, Chopra K, Rongzhu L, Kulkarni SK (2011) Protective effect of curcumin and its combination with piperine (bioavailability enhancer) against haloperidol-associated neurotoxicity: cellular and neurochemical evidence. Neurotox Res 20:215–225
Blanchet PJ, Parent M, Rompré PH, Lévesque D (2012) Relevance of animal models to human tardive dyskinesia. Behav Brain Funct 8:1–9
Burger ME, Fachinetto R, Zeni G, Rocha JBT (2005) Ebselen attenuates haloperidol-induced orofacial dyskinesia and oxidative stress in rat brain. Pharmacol Biochem Behav 81:608–615
Cadet JL, Lohr JB (1989) Possible involvement of free radicals in neuroleptic-induced movement disorders: evidence from treatment of tardive dyskinesia with vitamin E. Ann NY Acad Sci 570:176–185
Casey DE (2000) Tardive dyskinesia: pathophysiology and animal models. J Clin Psychiat 61(suppl 4):5–9
Cheng YF, Paalzow LK (1992) Linear pharmacokinetics of haloperidol in the rat. Biopharm Drug Dispos 13:69–76
Chiu JA, Franklin RB (1996) Analysis and pharmacokinetics of olanzapine (LY170053) and two metabolites in rat plasma using reversed-phase HPLC with electrochemical detection. J Pharmaceut Biomed 14:609–615
Correll CU, Schenk EM (2008) Tardive dyskinesia and new antipsychotics. Curr Opin Psychiatr 21:151–156
Dahl SG (1986) Plasma level monitoring of antipsychotic drugs clinical utility. Clin Pharmacokinet 11:36–61
Daya RP, Tan ML, Sookram CD, Skoblenick K, Mishra RK (2011) Alpha-phenyl-N-tert-butylnitrone prevents oxidative stress in a haloperidol-induced animal model of tardive dyskinesia: investigating the behavioural and biochemical changes. Brain Res 1412:28–36
Egan MF, Hurd Y, Ferguson J, Bachus SE, Hamid EH, Hyde TM (1996) Pharmacological and neurochemical differences between acute and tardive vacuous chewing movements induced by haloperidol. Psychopharmacology 127:337–345
Elkashef AM, Wyatt RJ (1999) Tardive dyskinesia: possible involvement of free radicals and treatment with vitamin E. Schizophrenia Bull 25:731–740
Fachinetto R, Burger ME, Wagner C, Wondracek DC, Brito VB, Nogueira CW, Ferreira J, Rocha JBT (2005) High fat diet increases the incidence of orofacial dyskinesia and oxidative stress in specific brain regions of rats. Pharmacol Biochem Behav 81:585–592
Fachinetto R, Villarinho JG, Wagner C, Pereira RP, Ávila DS, Burger ME, Calixto JB, Rocha JBT, Ferreira J (2007a) Valeriana officinalis does not alter the orofacial dyskinesia induced by haloperidol in rats: role of dopamine transporter. Prog Neuro-Psychoph 31:1478–1486
Fachinetto R, Villarinho JG, Wagner C, Pereira RP, Puntel RL, Paixão MW, Braga AL, Calixto JB, Rocha JBT, Ferreira J (2007b) Diphenyl diselenide decreases the prevalence of vacuous chewing movements induced by fluphenazine in rats. Psychopharmacology 194:423–432
Fibiger HC, Lloyd KG (1984) Neurobiological substrates of tardive dyskinesia: the GABA hypothesis. Trends Neurosci 7:462–464
Flatow J, Buckley P, Miller BJ (2013) Meta-analysis of oxidative stress in schizophrenia. Biol Psychiat 74:400–409
Grover S, Kumar P, Singh K, Vikram V, Budhiraja RD (2013) Possible beneficial effect of peroxisome proliferator-activated receptor (PPAR)—α and γ agonist against a rat model of oral dyskinesia. Pharmacol Biochem Behav 111:17–23
Kapur S, VanderSpek SC, Brownlee BA, Nobrega JN (2003) Antipsychotic dosing in preclinical models is often unrepresentative of the clinical condition: a suggested solution based on in vivo occupancy. J Pharmacol Exp Ther 305:625–631
Kirkpatrick B, Miller BJ (2013) Inflammation and schizophrenia. Schizophrenia Bull 39:1174–1179
Lohr JB, Kuczenski R, Niculescu AB (2003) Oxidative mechanisms and tardive dyskinesia. CNS Drugs 17:47–62
Macêdo DS, de Oliveira GV, Gomes PXL, de Araújo FYR, de Souza CM, Vasconcelos SMM, de Barros Viana GS, de Sousa FCF, Carvalho AF (2011) B vitamins attenuate haloperidol-induced orofacial dyskinesia in rats: possible involvement of antioxidant mechanisms. Behav Pharmacol 22:674–680
Merrill RM, Lyon JL, Matiaco PM (2013) Tardive and spontaneous dyskinesia in the general population. BMC Psychiatry 13:152
Nade VS, Kawale LA, Yadav AV (2010) Protective effect of Morus alba leaves on haloperidol-induced orofacial dyskinesia and oxidative stress. Pharm Biol 48:17–22
Naidu PS, Singh A, Kulkarni SK (2002) Carvedilol attenuates neuroleptic-induced orofacial dyskinesia: possible antioxidant mechanisms. Brit J Pharmacol 136:193–200
Naidu PS, Singh A, Kaur P, Sandhir R, Kulkarni SK (2003a) Possible mechanism of action in melatonin attenuation of haloperidol-induced orofacial dyskinesia. Pharmacol Biochem Behav 74:641–648
Naidu PS, Singh A, Kulkarni SK (2003b) Quercetin, a bioflavinoid, attenuates haloperidol-induced orofacial dyskinesia. Neuropharmacology 44:1100–1106
Naidu PS, Singh A, Kulkarni SK (2003c) Effect of Withania somnifera root extract on haloperidol-induced orofacial dyskinesia: possible mechanisms of action. J Med Food 6:107–114
Naidu PS, Singh A, Kulkarni SK (2003d) Reversal of haloperidol-induced orofacial dyskinesia by quercetin, a bioflavinoid. Psychopharmacology 167:418–423
Nelson LA, McGuire JM, Hausafus SN (2003) Melatonin for the treatment of tardive dyskinesia. Ann Pharmacother 37:1128–1131
Olfson M, Blanco C, Liu S, Wang S, Correll CU (2012) National trends in the office-based treatment of children, adolescents, and adults with antipsychotics. Arch Gen Psychiat 69:1247–1256
Pathan AA, Mohan M, Kasture AS, Kasture SB (2011) Mucuna pruriens attenuates haloperidol-induced orofacial dyskinesia in rats. Nat Prod Res 25:764–771
Patil R, Hiray Y, Shinde S, Langade P (2012) Reversal of haloperidol-induced orofacial dyskinesia by Murraya koenigii leaves in experimental animals. Pharm Biol 50:691–697
Prigol M, Pinton S, Schumacher R, Nogueira CW, Zeni G (2010) Convulsant action of diphenyl diselenide in rat pups: measurement and correlation with plasma, liver and brain levels of compound. Arch Toxicol 84:373–378
Remington G (2007) Tardive dyskinesia: eliminated, forgotten, or overshadowed? Curr Opin Psychiatr 20:131–137
Rogoza RM, Fairfax DF, Henry P, N-Marandi S, Khan RF, Gupta SK, Mishra RK (2004) Electron spin resonance spectroscopy reveals alpha-phenyl-N-tert-butylnitrone spin-traps free radicals in rat striatum and prevents haloperidol-induced vacuous chewing movements in the rat model of human tardive dyskinesia. Synapse 54:156–163
Sachdev PS (2000) The current status of tardive dyskinesia. Aust Nz J Psychiat 34:355–369
Sachdev P, Saharov T, Cathcart S (1999) The preventative role of antioxidants (selegiline and vitamin E) in a rat model of tardive dyskinesia. Biol Psychiat 46:1672–1681
Sadan O, Bahat-Stromza M, Gilgun-Sherki Y, Atlas D, Melamed E, Offen D (2005) A novel brain-targeted antioxidant (AD4) attenuates haloperidol-induced abnormal movement in rats: implications for tardive dyskinesia. Clin Neuropharmacol 28:285–288
Saltz BL, Woerner MG, Kane JM, Lieberman JA, Alvir JMJ, Bergmann KJ, Blank K, Koblenzer J, Kahaner K (1991) Prospective study of tardive dyskinesia incidence in the elderly. J Amer Med Assoc 266:2402–2406
Sampath C, Haug K, Thanei S, Hamburger M, Derendorf H, Frye R, Butterweck V (2012) Pharmacokinetics of valerenic acid in rats after intravenous and oral administrations. Planta Med 78:575–581
Sarró S, Pomarol-Clotet E, Canales-Rodriguez EJ, Salvador R, Gomar JJ, Oritz-Gil J, Landin-Romero R, Vila-Rodriguez F, Blanch J, McKenna PJ (2013) Structural brain changes associated with tardive dyskinesia in schizophrenia. Brit J Psychiat 203:51–57
Singh A, Naidu PS, Kulkarni SK (2003) Possible antioxidant and neuroprotective mechanisms of FK506 in attenuating haloperidol-induced orofacial dyskinesia. Eur J Pharmacol 477:87–94
Soares-Weiser K, Maayan N, McGrath J (2011) Vitamin E for neuroleptic-induced tardive dyskinesia. Cochrane DB Syst Rev. doi:10.1002/14651858.CD000209.pub2
Sohal RS, Weindruch R (1996) Oxidative stress, caloric restriction, and aging. Science 273:59–63
Sookram C, Tan M, Daya R, Heffernan S, Mishra RK (2011) Curcumin prevents haloperidol-induced development of abnormal oro-facial movements: possible implications of Bcl-XL in its mechanism of action. Synapse 65:788–794
Teixeira A, Müller LG, Reckziegel P, Boufleur N, Pase CS, Villarinho JG, Fachinetto R, Ferreira J, Rocha JBT, Bürger ME (2011) Beneficial effects of an innovative exercise model on motor and oxidative disorders induced by haloperidol in rats. Neuropharmacology 60:432–438
Thaakur S, Himabindhu G (2009) Effect of alpha lipoic acid on the tardive dyskinesia and oxidative stress induced by haloperidol in rats. J Neural Transm 116:807–814
Thaakur SR, Jyothi B (2007) Effect of spirulina maxima on the haloperidol induced tardive dyskinesia and oxidative stress in rats. J Neural Transm 114:1217–1225
Turrone P, Remington G, Nobrega JN (2002) The vacuous chewing movement (VCM) model of tardive dyskinesia revisited: is there a relationship to dopamine D2 receptor occupancy? Neurosci Biobehav R 26:361–380
Turrone P, Remington G, Kapur S, Nobrega JN (2003) Differential effects of within-day continuous vs transient dopamine D2 receptor occupancy in the development of vacuous chewing movements (VCMs) in rats. Neuropsychopharmacol 28:1433–1439
West IC (2000) Radicals and oxidative stress in diabetes. Diabetic Med 17:171–180
Yamamoto BK, Raudensky J (2008) The role of oxidative stress, metabolic compromise, and inflammation in neuronal injury produced by amphetamine-related drugs of abuse. J Neuroimmune Pharm 3:203–217
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lister, J., Nobrega, J.N., Fletcher, P.J. et al. Oxidative stress and the antipsychotic-induced vacuous chewing movement model of tardive dyskinesia: evidence for antioxidant-based prevention strategies. Psychopharmacology 231, 2237–2249 (2014). https://doi.org/10.1007/s00213-014-3582-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-014-3582-6