Abstract
Aims/hypothesis
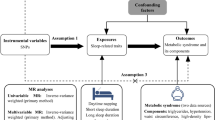
Short and long sleep duration are associated with increased risk of type 2 diabetes. We aimed to investigate whether genetic variants for fasting glucose or type 2 diabetes associate with short or long sleep duration and whether sleep duration modifies the association of genetic variants with these traits.
Methods
We examined the cross-sectional relationship between self-reported habitual sleep duration and prevalence of type 2 diabetes in individuals of European descent participating in five studies included in the Candidate Gene Association Resource (CARe), totalling 1,474 cases and 8,323 controls. We tested for association of 16 fasting glucose-associated variants, 27 type 2 diabetes-associated variants and aggregate genetic risk scores with continuous and dichotomised (≤5 h or ≥9 h) sleep duration using regression models adjusted for age, sex and BMI. Finally, we tested whether a gene × behaviour interaction of variants with sleep duration had an impact on fasting glucose or type 2 diabetes risk.
Results
Short sleep duration was significantly associated with type 2 diabetes in CARe (OR 1.32; 95% CI 1.08, 1.61; p = 0.008). Variants previously associated with fasting glucose or type 2 diabetes and genetic risk scores were not associated with sleep duration. Furthermore, no study-wide significant interaction was observed between sleep duration and these variants on glycaemic traits. Nominal interactions were observed for sleep duration and PPARG rs1801282, CRY2 rs7943320 and HNF1B rs4430796 in influencing risk of type 2 diabetes (p < 0.05).
Conclusions/interpretation
Our findings suggest that differences in habitual sleep duration do not mediate or modify the relationship between common variants underlying glycaemic traits (including in circadian rhythm genes) and diabetes.
Similar content being viewed by others
Introduction
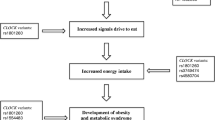
Several cross-sectional epidemiological studies have reported an association between short (<6 or <5 h/night) and long sleep duration (>9 h/night) with increased risk of impaired glucose tolerance (IGT) and/or type 2 diabetes, independent of BMI [1–6]. Prospective longitudinal studies suggest that this relationship is causal and that short or long sleep duration at baseline predicts subsequent development of type 2 diabetes [7–13].
In-laboratory studies of experimental sleep restriction confirm and extend these findings. Marked alterations in glucose metabolism, including decreased glucose tolerance and insulin sensitivity, were first demonstrated in 11 healthy young adults subjected to recurrent partial sleep restriction (4 h per night for six nights) [14]. In 20 healthy men, sleep restriction (5 h/night) for 1 week significantly reduced insulin sensitivity as measured by a hyperinsulinaemic–euglycaemic clamp [15]. Prolonged sleep restriction and concurrent circadian disruption (3 weeks of 5.6 h/24 h in recurring 28 h sleep/wake cycles) resulted in increased postprandial plasma glucose levels due to inadequate pancreatic insulin secretion [16].
The mechanistic links between sleep and glucose metabolism are poorly understood [17, 18]. It is not known whether the sleep duration–type 2 diabetes relationship reflects underlying shared genetic mechanisms, or whether habitual sleep duration is primarily a behavioural risk factor contributing to increased risk of diabetes. Evidence supporting the existence of a shared underlying genetic mechanism comes from Clock-deficient mice, which have disruption of both sleep duration and glucose metabolism [19], and from recent genome-wide association studies (GWAS) reporting that variants in two loci related to sleep, MTNR1B (encoding melatonin receptor 1B, one of two receptors for the sleep-promoting hormone melatonin) and CRY2 (encoding cryptochrome 2, a core clock gene), are associated with increased fasting glucose levels and/or risk of type 2 diabetes [20–23]. Recent studies have examined the association between MTNR1B type 2 diabetes risk variants and sleep disturbances, including sleep duration, but no association was observed [24, 25].
The objective of this study was to use a large sample of participants with European ancestry and with cross-sectional sleep and glycaemic trait measures to test the following: (1) whether previously established genetic variants for type 2 diabetes or fasting glucose or combined genetic risk scores are associated with habitual, self-reported sleep duration, which would suggest shared underlying causal mechanisms; or (2) whether habitual sleep duration modifies the association between genetic variants and type 2 diabetes or fasting glucose, which would provide information on the interaction of sleep habits with genetic susceptibility to type 2 diabetes.
Methods
Study sample
Participants were European American participants in the Candidate Gene Association Resource (CARe) study, which was comprised of five National Institutes of Health Heart, Lung and Blood Institute (NHLBI) cohort studies (Atherosclerosis Risk In Communities [ARIC], Coronary Artery Risk Development in Young Adults [CARDIA], Cardiovascular Health Study [CHS], Framingham Heart Study [FHS] and Multi-Ethnic Study of Atherosclerosis [MESA]) [26]. Study participants in the five original NHLBI studies gave informed consent and CARe study investigations were approved by the responsible institutional review boards.
The CARe study undertook genotyping of ∼50,000 single nucleotide polymorphisms (SNPs) in ∼2,000 cardiovascular candidate genes in European Americans using a gene-centric genotyping array, with the aim of identifying loci for complex traits measured in the NHLBI component studies. The study design and methods have been described previously [26]. In the cross-sectional analyses presented here, we included all subjects for whom type 2 diabetes status, fasting glucose and self-reported habitual sleep duration was ascertained within a 12 month period. Subjects were excluded if they had missing data for age, sex, BMI (calculated as weight in kilograms divided by square of height in metres), type 2 diabetes status or sleep duration. The total number of subjects included was 9,797 (1,474 type 2 diabetes cases and 8,323 controls). Overall, 4,323 individuals with genotyping data were excluded from cross-sectional analysis because of missing information on age (n = 34), BMI (n = 54), type 2 diabetes (n = 4,175) and/or sleep duration (n = 1,808). While the prevalence of type 2 diabetes did not differ significantly between subjects with and without sleep duration data, the average sleep duration was significantly longer (6 min) in subjects with type 2 diabetes than in subjects without (p < 0.05). This exclusion biases towards long sleep duration in the analyses presented here, and is expected to result in a slight underestimation of effect size for relationship between short sleep duration and type 2 diabetes.
Type 2 diabetes cases were defined based on an individual meeting at least one of the following criteria: (1) the American Diabetes Association (ADA) 2003 criteria [27]; (2) fasting (8 h or longer) glucose ≥7 mmol/l (≥126 mg/dl); (3) 2 h glucose ≥11.1 mmol/l (≥200 mg/dl) during an oral glucose tolerance test (OGTT); (4) use of glucose-lowering medications; (5) non-fasting plasma glucose >11.1 mmol/l (>200 mg/dl); (6) physician/self-report of diabetes, as previously described [28]. Cases were selected with age ≥25 years at the time of diagnosis or at exam visit. Controls within each study were individuals not classified as type 2 diabetes cases, with age at examination ≥25 years. For the ARIC and CHS studies with OGTT measures, controls with normal glucose tolerance (NGT) were defined as non-diabetic individuals with 2 h glucose <7.8 mmol/l (<140 mg/dl) during an OGTT.
Habitual sleep duration was assessed by questionnaires [29–31]. Usual sleep time was defined as the response to the following cohort-specific questions: for ARIC, the Sleep Heart Health Study (SHHS) [29], component of FHS and for MESA, ‘How many hours of sleep do you usually get at night (or your main sleep period) on weekdays or workdays?’; for CARDIA, [30] ‘During the past month, excluding naps, how many hours of actual sleep did you get at night (or day, if you work at night) on average?’; for CHS [31], ‘In a usual 24-hour period, how many hours do you spend sleeping during the night?’. Subjects reporting sleep duration ≤3 h or ≥14 h and reporting shift work were excluded. Clinical and sleep duration characteristics of the study populations are described in Table 1. Two questions on sleep medication were available for FHS SHHS (‘Do you take sleeping pills at least 1 day per week?’ and ‘How often do you take sleeping pills or other medication to help you sleep?’). In FHS SHHS and MESA, self-report or physician diagnosis of sleep apnoea was assessed by questionnaire based on the answers to the following questions: ‘Have you ever been told by a doctor that you have sleep apnea?’ (FHS SHHS) or: ‘Do you have sleep apnea or obstructive sleep apnea?’ (MESA).
Relationship between sleep duration and type 2 diabetes
The relation between sleep duration and type 2 diabetes was assessed in all five cohorts. Sleep duration was recorded to the nearest hour in ARIC, FHS SHHS, MESA and CHS and to the nearest half hour in a subset of CARDIA. The percentage of individuals with diabetes was examined in each of seven categories of self-reported sleep duration: 4, 5, 6, 7, 8, 9, 10 h or more (for this analysis, CARDIA half-hour values were rounded up to the next hour; Fig. 1). Association between type 2 diabetes and dichotomised short sleep duration (≤5 h) or long sleep duration (≥9 h) was assessed by logistic regression analysis relative to normal sleep duration (defined as sleep duration of 6, 7 or 8 h, categories which fall within one SD from the mean observed in both type 2 diabetes cases and controls; Table 1), with all analyses adjusted for age, sex and BMI. Association analyses were performed in R version 2.14.0 (http://www.r-project.org).
Relationship between sleep duration and type 2 diabetes in the CARe cohorts. The CARe study consists of ARIC (a), FHS (b), CARDIA (c), CHS (d), MESA (e) and combined study (f) with correlation between sleep duration and type 2 diabetes of r 2 = 0.6031, 0.1874, 0.6969, 0.6923, 0.7345 and 0.8451, respectively. Scatter plots represent the association between average sleep duration and percentage of individuals with diabetes, adjusted for age, sex and BMI, in the five European American studies. Sleep duration was categorised into bins of 4, 5, 6, 7, 8, 9 and 10–13 h
Genotyping, quality control and single nucleotide polymorphism selection
Genotyping and quality control for >53,000 SNPs from 2,000 cardiovascular candidate genes were performed by the central analysis group of the CARe consortium as previously described [32]. Briefly, the Illumina Itmat-Broad-CARe (IBC) SNP array was used for genotyping of all samples from the study and SNPs were clustered into genotypes using the Illumina Bead Studio software (Illumina, San Diego, CA, USA). Quality control was performed both for individual samples and individual SNPs. Samples with <90% individual call rate and non-European ancestry, as determined by principal component analysis using Eigenstrat [33], and SNPs with <95% call rate were removed.
To evaluate as many GWAS-identified genetic variants for type 2 diabetes and fasting glucose as possible that were present on the array, we selected the closest proxy on the IBC chip for previously reported (prior to January 2012) genome-wide significant genetic variants associated with fasting glucose levels [21] or risk of type 2 diabetes [34] in Europeans based on linkage disequilibrium patterns in the HapMap 2 white residents of European ancestry from Utah, USA (Centre d’Etude du Polymorphisme [Utah residents with northern and western European ancestry; CEU]) sample with pair-wise r 2 > 0.5 (ESM Tables 1, 2). For the fasting glucose genetic risk score, we also included type 2 diabetes variants associated with fasting glucose in the Meta-Analyses of Glucose and Insulin-related Traits Consortium (MAGIC) meta-analysis with p < 10−3 [34]. Sixteen variants for fasting glucose and 27 for type 2 diabetes were available with differing statistical power to detect glycaemic trait associations (ESM Tables 1, 2). The content on the array is biased towards gene regions and, more specifically, towards candidate genes for cardiovascular disease [32], therefore genotypes for 15 additional GWAS-identified glycaemic trait variants were not available. Nonetheless, SNPs on the IBC array capture common association signals with the strongest known genetic effects for both fasting glucose and type 2 diabetes in European populations because index SNPs at loci known by 2009 were prioritised during array design.
Statistical analysis
Genetic association analysis for continuous and dichotomised sleep duration was performed separately in each study using linear or logistic regression analysis in the software package PLINK [35]. Each SNP or genetic risk score was coded in an additive manner and additional adjustment for age, sex, BMI and type 2 diabetes status was performed. Meta-analysis was performed using a fixed-effect, inverse-variance approach as implemented in the program METAL [36]. Study-wide significance was assessed after Bonferroni correction for the number of independent hypotheses tested (33 hypotheses including six association signals for fasting glucose only, 17 signals for type 2 diabetes only and 10 overlapping signals; p < 0.0015).
SNP × sleep duration interaction analysis for fasting glucose in non-diabetic individuals was performed using a linear regression model with SNPs coded in an additive model, including covariates age, sex, BMI and sleep duration coded as a dichotomous/continuous variable. SNP × sleep duration interaction analysis for type 2 diabetes in each case–control sample was performed using logistic regression with SNPs coded in an additive genetic model with adjustment for age, sex, BMI and sleep duration coded as a dichotomous/continuous variable.
For genetic risk score (GRS) analyses, in each individual we generated an average unweighted multi-SNP genotypic risk score from 27 genome-wide significant type 2 diabetes SNPs, by summing the number of risk alleles for type 2 diabetes across the selected loci and dividing by the number of non-missing SNPs and a weighted genotypic risk score by weighting each risk allele by its previously reported effect size. We evaluated the contribution of both GRSs to type 2 diabetes in logistic regression models adjusting for age, sex and BMI. Furthermore, a GRS of 16 fasting glucose SNPs was calculated as described above. The contribution of the GRSs to fasting glucose was evaluated in linear regression models adjusting for age, sex and BMI. We report results for the more conservative unweighted risk score, but weighting risk variants by previously reported effect sizes did not substantially alter the results (data not shown).
Results
Short sleep duration is significantly associated with prevalence of type 2 diabetes in CARe
We examined the association between sleep duration and risk of type 2 diabetes using a logistic regression model adjusting for age, sex and BMI for each dataset in CARe. Short sleep duration (5 h or less) was associated with increased risk of type 2 diabetes relative to normal sleep duration (6–8 h) after adjustment for age, sex and BMI (OR [95% CI] 1.32 [1.08, 1.61]; p = 0.0077; Table 2; Fig. 1). Long sleep duration (9 h or more) was not significantly associated with prevalent type 2 diabetes after adjustment for age, sex and BMI (OR [95% CI] 1.14 [0.94, 1.38]; p = 0.19; Table 2). Additional adjustment for sleep apnoea did not substantially alter association results in the FHS SHHS and MESA studies in which sleep apnoea status was available (ESM Table 3).
In a subset of the ARIC and CHS cohorts with 2 h glucose measured during an OGTT, the association of short sleep with prevalent type 2 diabetes was stronger (OR [95% CI] 1.80 [1.26, 2.58]; p = 0.0013; ESM Table 4). No significant association of sleep duration of 9 h or more with increased prevalent type 2 diabetes (OR [95% CI] 1.15 [0.81, 1.64]; p = 0.44) was seen. Neither short nor long sleep duration was associated with IGT (ESM Table 4).
Associations of genetic variants and risk scores with fasting glucose or type 2 diabetes
We confirmed study-wide significant association with fasting glucose for the fasting glucose GRS (β [SE] 0.014 [0.036] mmol/l; p = 2.56 × 10−12) and MTNR1B, G6PC2, GCK, GCKR, TCF7L2 and SLC30A8 variants. Nominal associations were confirmed at six additional loci (ESM Table 5). We also confirmed study-wide significant association with risk of type 2 diabetes for the type 2 diabetes GRS (OR [95%CI] 1.10 [1.08, 1.12]; p = 3.96 × 10−22), TCF7L2, CDKAL1 and IGF2BP2 variants (ESM Table 6), with nominal associations for three additional loci. Notably, we did not observe association of MTNR1B rs10830963 G with prevalent type 2 diabetes, likely due to low power in the sample (38%; ESM Table 2), although the direction of effect was consistent with increased risk.
Associations of genetic variants for fasting glucose or type 2 diabetes with short or long sleep duration
We tested for association of previously reported genetic variants for fasting glucose or type 2 diabetes (including at loci harbouring circadian genes MTNR1B [rs10830963] and CRY2 [rs7933420; a proxy with r 2 = 1.00 in CEU 1000G for rs11605924]) with continuous sleep duration and dichotomised short or long sleep duration adjusting for age, sex and BMI. Association for validated type 2 diabetes risk variants with sleep duration in each cohort was examined in the entire case–control population (with additional adjustment for type 2 diabetes status), as well as separately in diabetic and non-diabetic individuals. No variant demonstrated study-wide significant association with sleep duration (Table 3 and ESM Tables 7–9). Nominally significant associations were seen for the ADAMTS9 region rs4607103 type 2 diabetes risk allele with longer average sleep duration and for the FADS1 rs1535 fasting glucose raising allele and NOTCH2 region rs10923931 type 2 diabetes risk allele with shorter average sleep duration (p = 0.023, p=0.032 and p = 0.037, respectively; ESM Table 7). The PPARG rs1801282 G allele, which is protective for type 2 diabetes, was also nominally associated with short sleep duration (p = 0.011; ESM Table 8). A genetic risk score of 13 fasting glucose-raising alleles in non-diabetic individuals or of 27 type 2 diabetes risk alleles in all samples did not significantly associate with either short or long sleep duration (p > 0.05; Table 3). No difference was seen in models re-analysed without adjustment for BMI (data not shown).
Sleep duration does not modify the association of genetic variants with fasting glucose or type 2 diabetes
To examine whether sleep duration modifies the effect of key variants on fasting glucose, we tested for interaction between sleep duration and each SNP in influencing fasting glucose levels in non-diabetic individuals (n ∼ 8,219). No significant SNP × average sleep duration interaction was observed (p > 0.05 for all SNPs; ESM Table 5). However, tests of interaction between SNPs and dichotomised sleep duration in influencing fasting glucose levels identified a PPARG rs1801282 × short sleep interaction (n = 7,284; ESM Table 10 and ESM Fig. 1) and an HMGA2 rs17179453 × long sleep interaction (n = 7,266; ESM Table 11 and ESM Fig. 1).
We next performed SNP × sleep duration interaction analyses for type 2 diabetes in the entire sample (n ∼ 9,920 subjects), but again, no study-wide significant interaction was observed. Nominally significant interactions were observed between SNPs at the PPARG, CRY2 and HNF1B loci and sleep duration (p < 0.05; ESM Fig. 2 and ESM Table 6) although the overall type 2 diabetes association signal at each locus was not significant. In subset analyses of SNP interaction with dichotomised short sleep duration, both the CRY2 and PPARG SNP × behaviour interactions remained nominally significant (ESM Fig. 3 and ESM Tables 12, 13).
Discussion
In five CARe cohorts comprising a total of >9,000 individuals of European ancestry, we found that short habitual sleep duration is significantly associated with increased prevalence of type 2 diabetes. However, we also found that previously established genetic variants for type 2 diabetes or for fasting glucose, either singly or in aggregate, are not associated with habitual, self-reported sleep duration, suggesting little shared genetic causal mechanisms. In addition, habitual sleep duration does not significantly modify the association between genetic variants and type 2 diabetes or fasting glucose, suggesting that it is not a behaviour that influences the effect of known genetic variants on glycaemic traits.
Our results confirm and extend the association between self-reported short sleep duration and risk of type 2 diabetes observed in previous studies [1, 3–10, 13, 16–18] or in subsets of the current study [2, 37]. While our entire dataset considered individuals with both NGT and IGT as being non-diabetic, restricting controls to individuals with NGT in a subset of our sample showed a greater effect of short sleep duration on type 2 diabetes risk, as previously reported [2]. We did not replicate the relationship between long sleep duration and diabetes, although the direction of effect was consistent with previous reports [8] and a meta-analysis of our study with available data from two previous cross-sectional studies [1, 6] was significant (OR 1.29 [1.10, 1.51], p = 0.0015).
Our study is large and has >99% power to detect previously reported associations between short and long sleep duration and diabetes, and has >80% power to detect SNP associations of >5 min change in average sleep duration, which might mediate association with type 2 diabetes at study-wide significance (Quanto version 1.2: http://hydra.usc.edu/gxe/). Some limiting features of the phenotype data reduce power to detect true associations. First, an assessment of sleep duration in CARe was based on self-report, which may misclassify sleep duration when compared with objective measures using actigraphy or polysomnography [38, 39]. Second, the questions used to determine sleep duration differed slightly between the cohorts (in estimate of weekday vs average weekly sleep duration); however, a post hoc sub-analysis of cohorts limited to weekday sleep duration found similar results (not shown). Third, our study only addresses sleep duration, which may be a heterogeneous, cumulative outcome dependent on genetic, environmental, social and workplace factors in addition to other sleep disturbances and circadian misalignment. Fourth, sleep duration and its relationship with type 2 diabetes may be influenced by disorders such as sleep apnoea or depression, or by use of sleep medications. However, these data were not available from a large enough population to be included as covariates in association analyses across all datasets. Finally, the analyses presented here are based on cross-sectional observations, and studies with longitudinal measurement of sleep duration and incident diabetes outcome may yield greater insights into subtle causal genetic effects underlying both traits.
We did not identify significant association of known fasting glucose or type 2 diabetes genetic variants with sleep duration, either singly or in aggregate, suggesting that sleep duration and type 2 diabetes do not share causal genetic pathways. In addition to SNPs at MTNR1B, a gene associated with one of two receptors for the circadian and sleep-promoting hormone melatonin, and CRY2, a core circadian clock gene, we tested several glycaemic trait loci harbouring genes that have been implicated in circadian rhythms including PROX1 [40] and PPARG [41, 42]. Circadian regulation is one of two major physiological processes contributing to sleep [43]. However, shared genetic determinants between sleep duration and diabetes in the circadian pathway were not identified in our study, perhaps because circadian processes regulate timing of sleep/wake propensity and therefore only have an indirect impact on sleep duration. Our findings are consistent with those of previous studies [24, 25] and with recent observations that type 2 diabetes and glucose SNPs primarily act in peripheral tissues to influence insulin secretion or insulin resistance [44]. No robust, genome-wide significant associations for sleep duration have yet been reported so we could not use a Mendelian randomisation genetic approach to evaluate the causal role of sleep duration in influencing risk of type 2 diabetes.
Our results also suggest that sleep duration does not strongly modify the association of genetic variants with fasting glucose or type 2 diabetes. Nominal interactions were seen with PPARG, CRY2 and HNF1B SNPs, but the impact of sleep duration on type 2 diabetes risk differed by risk genotypes across the genetic loci. For PPARG and HNF1B SNPs, carriers of the diabetic risk allele had blunted association between sleep duration and risk of type 2 diabetes as compared with non-carriers, whereas for the CRY2 SNP, short sleepers carrying the glucose-raising allele showed greater risk of type 2 diabetes than non-carriers. Since CRY2 variants may alter the biological clock and influence the timing of endogenous rhythms, modification of the association to risk of type 2 diabetes by sleep duration or sleep and wake timing is an attractive hypothesis that warrants future validation using objectively assessed sleep duration and timing measures in larger study samples.
In summary, while short sleep duration is associated with increased risk of type 2 diabetes in the CARe study, sleep duration does not mediate or significantly modify the association of genetic risk variants with type 2 diabetes or fasting glucose. Improvement of sleep duration habits might thus influence glycaemic trait outcomes equally across individuals regardless of an individual’s genetic risk of type 2 diabetes.
Abbreviations
- ARIC:
-
Atherosclerosis Risk In Communities
- BMI:
-
Body Mass Index
- CARDIA:
-
Coronary Artery Risk Development in Young Adults
- CARe:
-
Candidate Gene Association Resource
- CEU:
-
Centre d’Etude du Polymorphisme (Utah residents with northern and western European ancestry)
- CHS:
-
Cardiovascular Health Study
- CI:
-
Confidence interval
- FHS:
-
Framingham Heart Study
- GRS:
-
Genetic risk score
- GWAS:
-
Genome-wide association studies
- IBC:
-
Illumina Itmat-Broad-CARe
- IGT:
-
Impaired glucose tolerance
- MAGIC:
-
Meta-Analyses of Glucose and Insulin-related traits Consortium
- MESA:
-
Multi-Ethnic Study of Atherosclerosis
- NGT:
-
Normal glucose tolerance
- NHLBI:
-
National Institutes of Health Heart, Lung and Blood Institute
- OGTT:
-
Oral glucose tolerance test
- OR:
-
Odds ratio
- SHHS:
-
Sleep Heart Health Study
- SNP:
-
Single nucleotide polymorphism
References
Chaput JP, Despres JP, Bouchard C, Tremblay A (2007) Association of sleep duration with type 2 diabetes and impaired glucose tolerance. Diabetologia 50:2298–2304
Gottlieb DJ, Punjabi NM, Newman AB et al (2005) Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med 165:863–867
Jennings JR, Muldoon MF, Hall M, Buysse DJ, Manuck SB (2007) Self-reported sleep quality is associated with the metabolic syndrome. Sleep 30:219–223
Knutson KL, Ryden AM, Mander BA, van Cauter E (2006) Role of sleep duration and quality in the risk and severity of type 2 diabetes mellitus. Arch Intern Med 166:1768–1774
Tasali E, Leproult R, Spiegel K (2009) Reduced sleep duration or quality: relationships with insulin resistance and type 2 diabetes. Prog Cardiovasc Dis 51:381–391
Tuomilehto H, Peltonen M, Partinen M et al (2008) Sleep duration is associated with an increased risk for the prevalence of type 2 diabetes in middle-aged women – The FIN-D2D survey. Sleep Med 9:221–227
Ayas NT, White DP, Al-Delaimy WK et al (2003) A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care 26:380–384
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA (2010) Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 33:414–420
Gangwisch JE, Heymsfield SB, Boden-Albala B et al (2007) Sleep duration as a risk factor for diabetes incidence in a large U.S. sample. Sleep 30:1667–1673
Hayashino Y, Fukuhara S, Suzukamo Y, Okamura T, Tanaka T, Ueshima H (2007) Relation between sleep quality and quantity, quality of life, and risk of developing diabetes in healthy workers in Japan: the High-risk and Population Strategy for Occupational Health Promotion (HIPOP-OHP) Study. BMC Public Health 7:129
Mallon L, Broman JE, Hetta J (2005) High incidence of diabetes in men with sleep complaints or short sleep duration: a 12-year follow-up study of a middle-aged population. Diabetes Care 28:2762–2767
Nilsson PM, Roost M, Engstrom G, Hedblad B, Berglund G (2004) Incidence of diabetes in middle-aged men is related to sleep disturbances. Diabetes Care 27:2464–2469
Yaggi HK, Araujo AB, McKinlay JB (2006) Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care 29:657–661
Spiegel K, Leproult R, van Cauter E (1999) Impact of sleep debt on metabolic and endocrine function. Lancet 354:1435–1439
Buxton OM, Pavlova MK, Reid E et al (2008) Sleep restriction for 1 week reduces insulin sensitivity in healthy men. Diabetes 59:2126–2133
Buxton OM, Cain SW, O’Connor SP et al (2012) Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci Transl Med 4:129–143
Knutson KL (2010) Sleep duration and cardiometabolic risk: a review of the epidemiologic evidence. Best Pract Res Clin Endocrinol Metab 24:731–743
Punjabi NM (2009) Do sleep disorders and associated treatments impact glucose metabolism? Drugs 69(Suppl 2):13–27
Turek FW, Joshu C, Kohsaka A et al (2005) Obesity and metabolic syndrome in circadian Clock mutant mice. Science 308:1043–1045
Bouatia-Naji N, Bonnefond A, Cavalcanti-Proenca C et al (2009) A variant near MTNR1B is associated with increased fasting plasma glucose levels and type 2 diabetes risk. Nat Genet 41:89–94
Dupuis J, Langenberg C, Prokopenko I et al (2010) New genetic loci implicated in fasting glucose homeostasis and their impact on type 2 diabetes risk. Nat Genet 42:105–116
Lyssenko V, Nagorny CL, Erdos MR et al (2009) Common variant in MTNR1B associated with increased risk of type 2 diabetes and impaired early insulin secretion. Nat Genet 41:82–88
Prokopenko I, Langenberg C, Florez JC et al (2009) Variants in MTNR1B influence fasting glucose levels. Nat Genet 41:77–81
Liu C, Wu Y, Li H et al (2010) MTNR1B rs10830963 is associated with fasting plasma glucose, HbA1C and impaired beta-cell function in Chinese Hans from Shanghai. BMC Med Genet 11:59
Olsson L, Pettersen E, Ahlbom A, Carlsson S, Midthjell K, Grill V (2011) No effect by the common gene variant rs10830963 of the melatonin receptor 1B on the association between sleep disturbances and type 2 diabetes: results from the Nord-Trondelag Health Study. Diabetologia 54:1375–1378
Musunuru K, Lettre G, Young T et al (2010) Candidate gene association resource (CARe): design, methods, and proof of concept. Circ Cardiovasc Genet 3:267–275
Association: AD (2004) Diagnosis and classification of diabetes mellitus. Diabetes Care 27(Suppl 1):S5–S10
Saxena R, Elbers CC, Guo Y et al (2012) Large-scale gene-centric meta-analysis across 39 studies identifies type 2 diabetes loci. Am J Hum Genet 90:410–425
Quan SF, Howard BV, Iber C et al (1997) The Sleep Heart Health Study: design, rationale, and methods. Sleep 20:1077–1085
Lauderdale DS, Knutson KL, Yan LL et al (2006) Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol 164:5–16
Fried LP, Borhani NO, Enright P et al (1991) The Cardiovascular Health Study: design and rationale. Ann Epidemiol 1:263–276
Keating BJ, Tischfield S, Murray SS et al (2008) Concept, design and implementation of a cardiovascular gene-centric 50 k SNP array for large-scale genomic association studies. PLoS One 3:e3583
Price AL, Patterson NJ, Plenge RM, Weinblatt ME, Shadick NA, Reich D (2006) Principal components analysis corrects for stratification in genome-wide association studies. Nat Genet 38:904–909
Voight BF, Scott LJ, Steinthorsdottir V et al (2010) Twelve type 2 diabetes susceptibility loci identified through large-scale association analysis. Nat Genet 42:579–589
Purcell S, Neale B, Todd-Brown K et al (2007) PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 81:559–575
Willer CJ, Li Y, Abecasis GR (2010) METAL: fast and efficient meta-analysis of genomewide association scans. Bioinformatics 26:2190–2191
Knutson KL, van Cauter E, Zee P, Liu K, Lauderdale DS (2011) Cross-sectional associations between measures of sleep and markers of glucose metabolism among subjects with and without diabetes: the Coronary Artery Risk Development in Young Adults (CARDIA) Sleep Study. Diabetes Care 34:1171–1176
Silva GE, Goodwin JL, Sherrill DL et al (2007) Relationship between reported and measured sleep times: the sleep heart health study (SHHS). J Clin Sleep Med 3:622–630
Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ (2008) Self-reported and measured sleep duration: how similar are they? Epidemiology 19:838–845
Dufour CR, Levasseur MP, Pham NH et al (2011) Genomic convergence among ERRalpha, PROX1, and BMAL1 in the control of metabolic clock outputs. PLoS Genet 7:e1002143
Kawai M, Rosen CJ (2010) PPARgamma: a circadian transcription factor in adipogenesis and osteogenesis. Nat Rev Endocrinol 6:629–636
Yang G, Jia Z, Aoyagi T, McClain D, Mortensen RM, Yang T (2012) Systemic PPARgamma deletion impairs circadian rhythms of behavior and metabolism. PLoS One 7:e38117
Borbely AA (1982) A two process model of sleep regulation. Hum Neurobiol 1:195–204
Morris AP, Voight BF, Teslovich TM et al (2012) Large-scale association analysis provides insights into the genetic architecture and pathophysiology of type 2 diabetes. Nat Genet 44:981–990
Acknowledgements
We thank CARe cohort study participants, and the genotyping and central CARe statistical analysis group at the Broad Institute (Cambridge, MA, USA) for generating IBC array genotypes and quality control filtering.
Funding
This study was conducted with support to RS and FAJLS from NIDDK NIH R21 (DK089378) and from Harvard Catalyst of the Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award 8UL1TR000170-05 and financial contributions from Harvard University and its affiliated academic healthcare centres). The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centres or the National Institutes of Health. CARe and SHHS are supported by the National Heart, Lung, and Blood Institute cooperative agreement U01HL53941 (Boston University), U01HL53916 (University of California, Davis), U01HL53934 (University of Minnesota), U01HL 53937 and U01HL63429 (Johns Hopkins University) and U01HL 63463 (Case Western Reserve University). The CHS was supported by NHLBI contracts HHSN268201200036C, HHSN268200800007C, N01HC55222, N01HC85079, N01HC85080, N01HC85081, N01HC85082, N01HC85083 and N01HC85086 and by NHLBI grants HL080295, HL087652 and HL105756, with additional contribution from the National Institute of Neurological Disorders and Stroke (NINDS). Additional support was provided through AG023629 from the National Institute on Aging (NIA). A full list of CHS principal investigators and institutions can be found at www.chs-nhlbi.org/pi.
Duality of interest
All authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
CARe investigators contributed to phenotype data collection in study cohorts ARIC (NMP), CARDIA (DSL), CHS (SAG), FHS (DJG, TC), MESA (PCZ) and SHHS (SR). FAJLS, SR and RS conceived the analysis. AT and JML conducted the statistical analysis. AT and RS drafted the initial version of the manuscript, upon which all co-authors commented. All co-authors helped interpret data and reviewed and edited the manuscript, before approving its submission.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
(PDF 86.5 kb)
ESM Table 2
(PDF 100 kb)
ESM Table 3
(PDF 56 kb)
ESM Table 4
(PDF 58 kb)
ESM Table 5
(PDF 74.4 kb)
ESM Table 6
(PDF 84.5 kb)
ESM Table 7
(PDF 86.2 kb)
ESM Table 8
(PDF 92 kb)
ESM Table 9
(PDF 95.6 kb)
ESM Table 10
(PDF 82 kb)
ESM Table 11
(PDF 90.1 kb)
ESM Table 12
(PDF 82.3 kb)
ESM Table 13
(PDF 73.7 kb)
ESM Fig. 1
(PDF 159 kb)
ESM Fig. 2
(PDF 179 kb)
ESM Fig. 3
(PDF 161 kb)
Rights and permissions
About this article
Cite this article
Tare, A., Lane, J.M., Cade, B.E. et al. Sleep duration does not mediate or modify association of common genetic variants with type 2 diabetes. Diabetologia 57, 339–346 (2014). https://doi.org/10.1007/s00125-013-3110-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-013-3110-y