Abstract
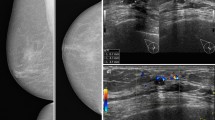
A case of invasive carcinoma of mixed papillary and not otherwise specified ductal type with areas of solid papillary ductal carcinomain situ (DCIS) is reported. The solid papillary areas were predominantly of low nuclear grade, but a small area of intermediate-grade solid papillary neoplasm was also seen within the tumor, together with an area suggestive of microinvasion. The massive regional nodal tumor load consisted of invasive papillary carcinoma and revertant low-grade solid papillary carcinoma with no myoepithelial cells around the circumscribed solid papillary areas. This is the first report of a solid papillary pattern simulating intraductal carcinoma in lymph nodes, and the first time that a solid papillary carcinoma is reported in association with invasive papillary carcinoma. The case suggests that mammary carcinomas with a solid papillary pattern may sometimes be of higher grade than usual, and do not always represent a DCIS, but may be invasive.
Similar content being viewed by others
References
Barsky SH, Bose S: Should LCIS be regarded as a heterogeneous disease? Breast J 5:407–412, 1999.
Barsky SH, Doberneck SA, Sternlicht MD, et al: “Revertant” DCIS in human axillary breast carcinoma metastases. J Pathol 183:188–194, 1997.
Buerger H, Otterbach F, Simon R, et al: Different genetic pathways in the evolution of invasive breast cancer are associated with distinct morphological subtypes. J Pathol 189:521–526, 1999.
Capella C, Eusebi V, Mann B, et al: Endocrine differentiation in mucoid carcinoma of the breast. Histopathology 4:613–630, 1980.
Cross AS, Azzopardi JG, Krausz T, et al: A morphological and immunohistochemical study of a distinctive variant of ductal carcinoma in situ of the breast. Histopathol 9:1–37, 1985.
Diest PJ van: Ductal carcinoma in situ in breast carcinogenesis. J Pathol 187:383–384, 1999.
Douglas-Jones AG, Gupta SK, Attanoos RL, et al: A critical appraisal of six modern classifications of ductal carcinoma in situ of the breast (DCIS): correlation with grade of associated invasive carcinoma. Histopathol 29: 97–409, 1996.
Ellis IO, Eslton CW, Poller DN: Ductal carcinoma in situ. In: Elston CW, Ellis IO (Eds) The Breast, Systemic Pathology, Volume 13, 3rd ed., pp 249–281. Churchill Livingstone, Edinburgh, 1998.
Elston CW, Ellis IO: Assessment of histological grade. In: Elston CW, Ellis IO (Eds) The Breast, Systemic Pathology, Volume 13, 3rd ed., pp 365–384. Churchill Livingstone, Edinburgh, 1998.
Lampejo OT, Barnes DM, Smith P, et al: Evaluation of infiltrating carcinomas with a DCIS component: correlation of the histologic type of the in situ component with the grade of the infiltrating component. Semin Diagn Pathol 11: 215–222, 1994
Lee AHS, Telfer TP, Millis RR: Metastatic breast carcinoma with appearance resembling micropapillary ductal carcinoma in situ. J Clin Pathol 48:380–382, 1995.
Maluf HM, Koerner FC: Solid papillary carcinoma of the breast. A form of intraductal carcinoma with endocrine differentiation frequently associated with mucinous carcinoma. Am J Surg Pathol 19:1237–1244, 1995.
Maluf HM, Zukerberg LR, Dickersin GR, et al: Spindle-cell argyrophilic mucin-producing carcinoma of the breast. Histological, ultrastructural, and immunohistochemical studies of two cases. Am J Surg Pathol 15:677–686, 1991.
ional Coordinating Group for Breast Screening Pathology Pathology reporting in breast cancer screening, 2nd ed., p65. NHS-BSP Publications, Sheffield, 1997.
Pinder SE, Elston CW, Ellis IO: Invasive carcinoma - usual histological types. In: Elston CW Ellis IO (Eds) The Breast, Systemic Pathology, Volume 13, 3rd ed., pp 283–337. Churchill Livingstone, Edinburgh, 1998.
Rosen PP, Oberman HA: Tumors of the mammary gland. Fascicle 7, 3rd series, p217. AFIP, Washington DC, 1993.
Roylance R, Gorman P, Harris W et al: Comparative genomic hybridisation of breast tumors stratified by histological grade reveals new insights into the biological progression of breast cancer. Cancer Res 59:1433–1436, 1999.
Saphir O: Mucinous carcinoma of the breast. Surg Gynecol Obstet 72:908–914, 1941.
Sternlicht MD, Kedeshian P, Shao ZM, et al: The human myoepithelial cell is a natural tumor suppressor. Clin Cancer Res 3:1949–1958, 1997.
Tsang WYW, Chan JKC: Endocrine ductal carcinoma in situ (EDCIS) of the breast. Am J Surg Pathol 20:921–943, 1996.
Yaziji H, Gown AM, Sneige N: Detection of stromal invasion in breast cancer: the myoepithalial markers. Adv Anat Pathol 7:100–109, 2000.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cserni, G. “Revertant” mammary solid papillary carcinoma in lymph node metastasis. Pathol. Oncol. Res. 8, 74–77 (2002). https://doi.org/10.1007/BF03033706
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF03033706