Abstract
Purpose
During the past few years, many oocyte insemination techniques, including microinjection, have evolved in the treatment of male-factor infertility. This preliminary study was designed to evaluate whether microdroplet insemination could be considered a reliable technique, especially for semen samples with male-factor defects. The first objective was to assess fertilization rates obtained by inseminating sibling oocytes using both the conventional IVF and the microdroplet method (Group 1). The second objective was to evaluate subsequent embryo development and pregnancy rates resulting from microdroplet insemination, in addition to formulating adequate sperm∶ oocyte ratios for various semen categories (Group 2). Four semen categories were studied including fresh normal sperm, frozen/thawed normal sperm, and male-factor sperm with one defect and two or three defects.
Results
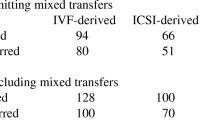
Group 1 consisted of 54 couples; no statistical significance was found in the fertilization rates between test tube and microdroplet insemination in all four semen categories. Based on these results, patients from Group 2 (48 couples) had their oocytes inseminated only in microdroplets with sperm:oocyte ratios ranging from 2000 to 10,000 motile sperm:1 oocyte. The average fertilization rate for male-factor sperm was 55%, with a 91% cleavage rate.
Conclusion
Higher fertilization rates were observed in the lowest range of sperm∶oocyte ratios (2000–4000∶1) for male-factor sperm with one defect and in the highest range (8000–10,000∶1) for male-factor sperm with two or three defects. Polyspermy occurred in only 0.4% of the oocytes inseminated. Microdroplet insemination is an alternative treatment for moderate to moderately severe male-factor infertility, establishing a bridge between conventional IVF and microinjection. With adequate sperm∶oocyte ratios, this technique allows the natural selection process of fertilization in vitro to take place, without the high incidence of polyspermy or mechanical damage frequently observed in assisted fertilization techniques.
Similar content being viewed by others
References
Cohen J, Edwards R, Fehilly C, Fishel S, Hewitt J, Purdy J, Rowland G, Steptoe P, Webster J: In vitro fertilization: A treatment for male infertility. Fertil Steril 1985;43:422–432
Awadalla SG, Friedman CI, Schmidt G, Chin N, Kim MH: In vitro fertilization and embryo transfer as a treatment for male factor infertility. Fertil Steril 1987;47:807–811
Trounson AO: The choice of the most appropriate microfertilization technique for human male factor infertility (submitted for publication), 1993
Malter HE, Cohen J: Partial zona dissection of the human oocyte: A nontraumatic method using micromanipulation to assist zona pellucida penetration. Fertil Steril 1989;51:139–148
Ng SC, Bongso A, Sathananthan H, Ratnam SS: Micromanipulation: Its relevance to human in vitro fertilization. Fertil Steril 1990;53:203–219
Palermo G, Joris H, Devroey P, Van Steirteghem AC: Pregnancies after intracytoplasmic injection of a single spermatozoon into an oocyte. Lancet 1992;340:17–18
Sakkas D, Lacham O, Gianaroli L, Trounson AO: Subzonal sperm microinjection in cases of severe male factor infertility and repeated in vitro fertilization failure. Fertil Steril 1992;57:1279–1288
Gianaroli L, Seracchioli R, Ferraretti AP, Trounson AO, Flamigni C, Bovicelli L: The successful use of human amniotic fluid for mouse embryo culture and human in vitro fertilization, embryo culture and transfer. Fertil Steril 1986;46:907–913
Whittingham DG: Culture of mouse ova. J Reprod Fertil (Suppl) 1971;14:7–21
World Health Organization: WHO Laboratory Manual for the Examination of Human Semen and Semen-Cervical Mucus Interaction. Cambridge, Cambridge University Press, 1992
Kruger TF, Menkveld R, Stander FSH, Lombard CJ, Van der Merwe JP, van Jyl JA, Smith K: Sperm morphologic features as a prognostic factor in in vitro fertilization. Fertil Steril 1986;46:1118–1123
Kruger TF, Acosta AA, Simmons KF, Swanson RJ, Matta JF, Veeck LL, Morshedi M, Brugo S: New method of evaluating sperm morphology with predictive value for human in vitro fertilization. Urology 1987;30:248–251
Mahadevan MM, Trounson AO: The influence of seminal characteristics on the success rate of human in vitro fertilization. Fertil Steril 1984;42:400–405
Ord T, Patrizio P, Marello E, Balmaceda JP, Asch RH: Minipercoll: A new method of semen preparation for IVF in severe male factor infertility. Hum Reprod 1990;5:987–989
Ng FLH, Yi Luii D, Baker HWG: Comparison of percoll, mini-percoll and swim-up methods for sperm preparation from abnormal semen samples. Hum Reprod 1992;7:261–266
Van Steirteghem AC, Nagy J, Joris H, Liu J, Staessen C, Smitz J, Wisanto A, Devroey P: High fertilization and implantation rates after intracytoplasmic sperm injection. Hum Reprod 1993;8:1061–1066
Palermo G, Joris H, Derde MP, Camus M, Devroey P, Van Steirteghem A: Sperm characteristics and outcome of human assisted fertilization by subzonal insemination and intracytoplasmic sperm injection. Fertil Steril 1993;59:826–835
Fishel S, Timson J, Lisi F, Rinaldi L: Evaluation of 225 patients undergoing subzonal insemination for the procurement of fertilization in vitro. Fertil Steril 1992;57:840–849
Dale B: Fertilization in Animals. London, Institute of Biological Studies in Biology, Edward Arnold, 1983
Dale B: Fertilization.In Human Physiology from Cellular Mechanisms to Integration, R Greger, H Koepchen, W Mommaerts (eds). Springer Verlag, Heidelberg, 1993
Tesarik J: Control of the fertilization process by the egg coat: How does it work in humans. J Assist Reprod Genet 1992;9:313–317
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Fiorentino, A., Magli, M.C., Fortini, D. et al. Sperm:Oocyte ratios in an in vitro fertilization (IVF) program. J Assist Reprod Genet 11, 97–103 (1994). https://doi.org/10.1007/BF02215995
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02215995