Abstract
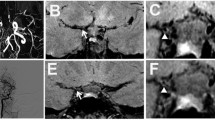
An 31-year-old female and a 32-year-old male had clinical signs and angiographical confirmation of adult Moyamoya disease (MMD). Bilateral carotid siphon (C1), middle cerebral artery (M1), and anterior cerebral artery (A1) stenoses were diagnosed by means of transcranial Doppler sonography (TCD) and visualized during angio Magnetic Resonance Imaging (angio-MRI). In the woman, a “rete mirabile’ of dilated and tortuous lenticulostriate arteries could be visualized during proton weighted and T1-weighted MRI sequences. CO2-dependent vasomotor reactivity was bilaterally reduced and completely exhausted in the territory of right middle cerebral artery in both patients. Cerebral perfusion reserve, defined as the ratio of cerebral blood flow (CBF) to cerebral blood volume (CBV) was assessed by SPECT, and was found to be dramatically reduced in the anterior region of the male patient. Both patients had bilateral small subcortical infarctions in the corona radiata. TCD and MRI are important noninvasive techniques for a preliminary diagnosis of Moyamoya disease. Infarctions in Moyamoya disease may be hemodynamically produced low-flow infarctions.
Similar content being viewed by others
References
Bruno A, HP Adams, J Biller, K Rezai, S Cornell, CA Aschenbrener. Cerebral infarction due to moyamoya disease in young adults. Stroke 19 (1988) 826–833
Buell U, H Braun, A Ferbert, H Stirner, C Weiller, EB Ringelstein: Combined SPECT imaging of regional cerebral blood flow (99mTc-Hexamethyl-Propyleneamine Oxime, HMPAO) and blood volume (99mTc-RBC) to assess regional cerebral perfusion reserve in patients with cerebrovascular disease. Nuclearmedicine 27 (1988) 51–56
Gibbs JM, RJS Wise, KL Leenders, T Jones: Evaluation of cerebral perfusion reserve in patients with carotid artery occlusion. Lancet II (1984) 310–314
Ringelstein EB, H Zeumer, D Angelou: The pathogenesis of strokes from internal carotid artery occlusion. Diagnostic and therapeutical implications. Stroke 14 (1983) 867–875
Ringelstein EB, C Sievers, S Ecker, PA Schneider, SM Otis. Noninvasive assessment of CO2-induced vasomotor response in normal individuals and patients with internal carotid artery occlusion. Stroke 19 (1988) 963–969
Ringelstein EB: A practical Guide to Transcranial Doppler Sonography. In: Noninvasive Imaging of Cerebrovascular Disease, Alan R. Liss, Inc. 1989
Suzuki J: Moyamoya disease. Springer, Berlin-Heidelberg-New York-Tokyo 1986
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Weiller, C., Müllges, W., Leibold, M. et al. Infarctions and non-invasive diagnosis in Moyamoya Disease: Two case report. Neurosurg. Rev. 14, 75–77 (1991). https://doi.org/10.1007/BF00338199
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00338199