Summary
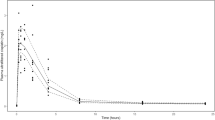
Carboplatin was given as a 30-min infusion to 11 ovarian cancer patients at doses of 170–500 mg/m2. The ages, weights, and creatinine clearances (Clcr) ranged from 44 to 75 years, from 44 to 74 kg, and from 32 to 101 ml/min, respectively. Plasma, plasma ultrafiltrate (PU), and urine samples were obtained at appropriate times for 96 h and were analyzed for platinum. The PU and urine were also analyzed for the parent compound by HPLC. In patients with a Clcr of about 60 ml/min or greater, carboplatin decayed biexponentially with a mean t1/2α of 1.6 h and a t1/2β of 3.0 h. The mean (±SD) residence time, total body clearance, and apparent volume of distribution were 3.5±0.4 h, 4.4±0.85 l/h, and 16±31l, respectively. Cmax and AUCinf values increased linearly with dose, and the latter values correlated better with the dose in mg than in mg/m2. No significant quantities of free, ultrafilterable, platinum-containing species other than the parent compound were found in plasma, but platinum from carboplatin became protein-bound and was slowly eliminated with a minimal t1/2 of 5 days. The major route of elimination was excretion via the kidneys. Patients with a Clcr of 60 ml/min or greater excreted 70% of the dose as the parent compound in the urine, with most of this occurring within 12–16 h. All of the platinum in 24-h urine was carboplatin, and only 2%–3% of the dosed platinum was excreted from 48 to 96 h. Patients with a Clcr of less than about 60 ml/min exhibited dose-disproportional increases in AUCinf and MRT values. The latter were inversely related to Clcr (r=-0.98). Over a dose range of 300–500 mg/m2, carboplatin exhibited linear, dose-independent pharmaco-kinetics in patients with a Clcr of about 60 ml/min or greater, but dose reductions are necessary for patients with mild renal failure.
Similar content being viewed by others
References
Calvert AH, Harland SJ, Newell DR, Siddik ZH, Jones AC, McElwain TJ, Raju S, Wiltshaw E, Smith IE, Baker JM, Peckham MJ, Harrap KR (1982) Early clinical studies with cis-diammine-1,1-cyclobutane dicarboxylate platinum II. Cancer Chemother Pharmacol 9: 140–147
Calvert AH, Harland SJ, Newell DR, Siddik ZH, Harrap KR (1985) Phase I studies with carboplatin at the Royal Marsen Hospital. Cancer Treat Rev 12 (Suppl A): 51–57
Colombo N, Speyer JL, Green Md, Wernz JC, Blum RH, Piccart M, Muggia FM (1986) Carboplatin (CBDCA) as salvage in ovarian cancer (OC): unpredictable myelotoxicity. Proc Am Soc Clin Oncol 5: 123
Curt GA, Grygiel JJ, Corden BJ, Ozols RF, Weiss RB, Tell DT, Myers CE, Collins JM (1983) A phase I and pharmacokinetic study of diamminecyclobutane-dicarboxylatoplatinum (NSC 241240). Cancer Res 43: 4470–4473
Egorin MJ, Van Echo DA, Tipping SJ, Olman EA, Whitacre MY, Thompson BW, Aisner J (1984) Pharmacokinetics and dose reduction of cis-diammine (1,1-cyclobutanedicarboxylato) platinum in patients with impaired renal function. Cancer Res 44: 5432–5438
Gaver RC, Deeb G (1986) High-performance liquid chromatographic procedures for the analysis of carboplatin in human plasma and urine. Cancer Chemother Pharmacol 16: 201–206
Gaver RC, George AM, Deeb G (1987) In vitro stability, plasma protein binding and blood cell partitioning of 14C-carboplatin. Cancer Chemother Pharmacol 20: 271–276
Gibaldi M, Perrier D (1982) Pharmacokinetics, 2nd edn. Marcel Dekker, New York
Harland SJ, Newell DR, Siddik ZH, Chadwick R, Calvert AH, Harrap KR (1984) Pharmacokinetics of cis-diammine-1,1-cyclobutane dicarboxylate platinum (II) in patients with normal and impaired renal function. Cancer Res 44: 1693–1697
Koeller JM, Trump DL, Tutsch KD, Earhart RH, Davis TE, Tormey DC (1986) Phase I clinical trial and pharmacokinetics of carboplatin (NSC 241240) by single monthly 30-minute infusion. Cancer 57(2): 222–225
Ostle B, Mensing R (1975) Statistics in research, 3rd edn. Iowa State University Press, Ames pp 165–242
Prescott P (1975) An approximate test for outliers in linear models. Technometrics 17: 129–132
Riegelman S, Collier P (1980) The application of statistical moment theory to the evaluation of in vivo dissolution time and absorption time. J Pharmacokinet Biopharm 8: 509–534
Rose WC, Schurig JE (1985) Preclinical antitumor and toxicologic profile of carboplatin. Cancer Treat Rev 12 (Suppl A): 1–19
Snedecor GW, Cochran WG (1980) Statistical methods, 7th edn. Iowa State University Press, Ames, pp 149–174
Van Echo DA, Egorin MJ, Whitacre MY, Olman EA, Aisner J (1984) Phase I clinical and pharmacologic trial of carboplatin daily for 5 days. Cancer Treat Rep 68 (9): 1103–1114
Woolley PV, Priego VM, Luc PVT, Rahman A, Schein PS (1984) Clinical pharmacokinetics of diammine [1,1-cyclobutanedicarboxylato (2)]0,0′-platinum (CBDCA) In: Hacker MF, Douple EB, Krakoff IH (eds): Platinum coordination complexes in cancer chemotherapy. Martinus Nijhoff, Boston, pp 82–89
Author information
Authors and Affiliations
Additional information
Supported in part by CA 16087, CRC-RR-96, AIFCR
Rights and permissions
About this article
Cite this article
Gaver, R.C., Colombo, N., Green, M.D. et al. The disposition of carboplatin in ovarian cancer patients. Cancer Chemother. Pharmacol. 22, 263–270 (1988). https://doi.org/10.1007/BF00273422
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00273422