Abstract
Stroke is defined as the acute onset of focal neurological disturbance arising due to a cerebrovascular cause, confirmed histopathologically or on imaging, where other causes have been excluded. Strokes may either be ischaemic (approximately 80% of cases) or haemorrhagic (20%). Although often thought of as a single disease, stroke represents the end stage of many different pathologies, each of which can result in cerebral ischaemia and/or haemorrhage. Therefore when investigating a stroke patient, investigations are performed to identify the underlying cause. Most cases of ischaemic stroke are caused by one of three pathologies: large vessel atherosclerotic disease (LVD), cerebral small vessel disease (SVD) or cardioembolism, although there are multiple rarer causes including cervical artery dissection. However, even with detailed investigation an underlying cause cannot be found in approximately a quarter of all ischaemic strokes. Haemorrhagic strokes are categorized according to the brain region they arise from; lobar or cortical haemorrhages are commonly caused by cerebral amyloid angiopathy, or an underlying structural lesion for example an arteriovenous malformation. Subcortical haemorrhages are usually associated with hypertension and believed to be often a manifestation of SVD.
This chapter will briefly outline the genetic basis of strokes in general, and highlight key examples of familial forms of stroke.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the twenty-first century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:2064–89. https://doi.org/10.1161/STR.0b013e318296aeca.
Flossmann E, Schulz U, Rothwell P. Systematic review of methods and results of studies of the genetic epidemiology of ischemic stroke. Stroke. 2004;35:212–27. https://doi.org/10.1161/01.STR.0000107187.84390.AA.
Meschia JF. Ischaemic stroke: one or several complex genetic disorders? Lancet Neurol. 2003;2:459.
Rubattu S, Volpe M, Kreutz R, et al. Chromosomal mapping of quantitative trait loci contributing to stroke in a rat model of complex human disease. Nat Genet. 1996;13:429–34. https://doi.org/10.1038/ng0896-429.
Bak S, Gaist D, Sindrup SH, et al. Genetic liability in stroke: a long-term follow-up study of Danish twins. Stroke. 2002;33:769–74.
Brass LM, Isaacsohn JL, Merikangas KR, Robinette CD. A study of twins and stroke. Stroke. 1992;23:221–3.
Kiely DK, P A W, L A C, et al. Familial aggregation of stroke. The Framingham Study. Stroke. 1993;24:1366–71. https://doi.org/10.1161/01.STR.24.9.1366.
Bevan S, Traylor M, Adib-Samii P, et al. Genetic heritability of ischemic stroke and the contribution of previously reported candidate gene and genomewide associations. Stroke. 2012;43:3161–7. https://doi.org/10.1161/STROKEAHA.112.665760.
Traylor M, Malik R, Nalls MA, et al. Genetic variation at 16q24.2 is associated with small vessel stroke. Ann Neurol. 2016;81(3):383–94. https://doi.org/10.1002/ana.24840.
Bellenguez C, Bevan S, Gschwendtner A, et al. Genome-wide association study identifies a variant in HDAC9 associated with large vessel ischemic stroke. Nat Genet. 2012;44:328–33. https://doi.org/10.1038/ng.1081.
Traylor M, Farrall M, Holliday EG, et al. Genetic risk factors for ischaemic stroke and its subtypes (the METASTROKE collaboration): a meta-analysis of genome-wide association studies. Lancet Neurol. 2012;11:951–62. https://doi.org/10.1016/S1474-4422(12)70234-X.
Neurology Working Group of the Cohorts for Heart and Aging Research in Genomic Epidemiology (CHARGE) Consortium, Stroke Genetics Network (SiGN), International Stroke Genetics Consortium (ISGC). Identification of additional risk loci for stroke and small vessel disease: a meta-analysis of genome-wide association studies. Lancet Neurol. 2016;15:695–707. https://doi.org/10.1016/S1474-4422(16)00102-2.
Traylor M, Mäkelä K-M, Kilarski LL, et al. A novel MMP12 locus is associated with large artery atherosclerotic stroke using a genome-wide age-at-onset informed approach. PLoS Genet. 2014;10:e1004469. https://doi.org/10.1371/journal.pgen.1004469.
Woo D, Falcone GJ, Devan WJ, et al. Meta-analysis of genome-wide association studies identifies 1q22 as a susceptibility locus for intracerebral hemorrhage. Am J Hum Genet. 2014;94:511–21. https://doi.org/10.1016/j.ajhg.2014.02.012.
Tan RYY, Markus HS. Monogenic causes of stroke: now and the future. J Neurol. 2015;262(12):2601–16. https://doi.org/10.1007/s00415-015-7794-4.
Joutel A, Haddad I, Ratelade J, Nelson MT. Perturbations of the cerebrovascular matrisome: a convergent mechanism in small vessel disease of the brain? J Cereb Blood Flow Metab. 2016;36:143–57. https://doi.org/10.1038/jcbfm.2015.62.
Tan RYY, Traylor M, Rutten-Jacobs L, Markus HS. New insights into mechanisms of small vessel disease stroke from genetics. Clin Sci. 2017;131(7):515–31.
Joutel A, Corpechot C, Ducros A, et al. Notch3 mutations in CADASIL, a hereditary adult-onset condition causing stroke and dementia. Nature. 1996;383:707–10. https://doi.org/10.1038/383707a0.
Fukutake T. Cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy (CARASIL): from discovery to gene identification. J Stroke Cerebrovasc Dis. 2011;20:85–93. https://doi.org/10.1016/j.jstrokecerebrovasdis.2010.11.008.
Verdura E, Hervé D, Scharrer E, et al. Heterozygous HTRA1 mutations are associated with autosomal dominant cerebral small vessel disease. Brain. 2015;138(Pt 8):2347–58. https://doi.org/10.1093/brain/awv155.
Nozaki H, Kato T, Nihonmatsu M, et al. Distinct molecular mechanisms of HTRA1 mutants in manifesting heterozygotes with CARASIL. Neurology. 2016;86:1964–74. https://doi.org/10.1212/WNL.0000000000002694.
Bugiani M, Kevelam SH, Bakels HS, et al. Cathepsin A-related arteriopathy with strokes and leukoencephalopathy (CARASAL). Neurology. 2016;87(17):1777–86. https://doi.org/10.1212/WNL.0000000000003251.
DiFrancesco JC, Novara F, Zuffardi O, et al. TREX1 C-terminal frameshift mutations in the systemic variant of retinal vasculopathy with cerebral leukodystrophy. Neurol Sci. 2014;36(2):323–30. https://doi.org/10.1007/s10072-014-1944-9.
French CR, Seshadri S, Destefano AL, et al. Mutation of FOXC1 and PITX2 induces cerebral small-vessel disease. J Clin Invest. 2014;124:4877–81. https://doi.org/10.1172/JCI75109.
Zhou Q, Yang D, Ombrello AK, et al. Early-onset stroke and vasculopathy associated with mutations in ADA2. N Engl J Med. 2014;370:911–20. https://doi.org/10.1056/NEJMoa1307361.
Jenkinson EM, Rodero MP, Kasher PR, et al. Mutations in SNORD118 cause the cerebral microangiopathy leukoencephalopathy with calcifications and cysts. Nat Genet. 2016;48(10):1185–92. https://doi.org/10.1038/ng.3661.
Mitsias P, Levine SR. Cerebrovascular complications of Fabry’s disease. Ann Neurol. 1996;40:8–17. https://doi.org/10.1002/ana.410400105.
Chassaing N, Martin L, Calvas P, et al. Pseudoxanthoma elasticum: a clinical, pathophysiological and genetic update including 11 novel ABCC6 mutations. J Med Genet. 2005;42:881–92. https://doi.org/10.1136/jmg.2004.030171.
Gutmann DH, Ferner RE, Listernick RH, et al. Neurofibromatosis type 1. Nat Rev. Dis Prim. 2017;3:17004. https://doi.org/10.1038/nrdp.2017.4.
Buoni S, Molinelli M, Mariottini A, et al. Homocystinuria with transverse sinus thrombosis. J Child Neurol. 2001;16:688–90. https://doi.org/10.1177/088307380101600913.
Renard D, Miné M, Pipiras E, et al. Cerebral small-vessel disease associated with COL4A1 and COL4A2 gene duplications. Neurology. 2014;83:1029–31. https://doi.org/10.1212/WNL.0000000000000769.
Revesz T, Holton JL, Lashley T, et al. Genetics and molecular pathogenesis of sporadic and hereditary cerebral amyloid angiopathies. Acta Neuropathol. 2009;118:115–30. https://doi.org/10.1007/s00401-009-0501-8.
Vidal R, Frangione B, Rostagno A, et al. A stop-codon mutation in the BRI gene associated with familial British dementia. Nature. 1999;399:776–81. https://doi.org/10.1038/21637.
Govani FS, Shovlin CL. Hereditary haemorrhagic telangiectasia: a clinical and scientific review. Eur J Hum Genet. 2009;17:860–71. https://doi.org/10.1038/ejhg.2009.35.
Perrone RD, Malek AM, Watnick T. Vascular complications in autosomal dominant polycystic kidney disease. Nat Rev. Nephrol. 2015;11:589–98. https://doi.org/10.1038/nrneph.2015.128.
Fischer A, Zalvide J, Faurobert E, et al. Cerebral cavernous malformations: from CCM genes to endothelial cell homeostasis. Trends Mol Med. 2013;19:302–8. https://doi.org/10.1016/j.molmed.2013.02.004.
Weitz NA, Lauren CT, Behr GG, et al. Clinical spectrum of capillary malformation-arteriovenous malformation syndrome presenting to a pediatric dermatology practice: a retrospective study. Pediatr Dermatol. 2015;32:76–84. https://doi.org/10.1111/pde.12384.
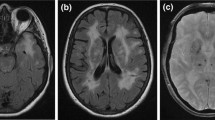
O’Sullivan M, Jarosz JM, Martin RJ, et al. MRI hyperintensities of the temporal lobe and external capsule in patients with CADASIL. Neurology. 2001;56:628–34.
Bellingham AJ. The sickling process in relation to clinical manifestations. J Clin Pathol. 1974;8:23–5.
Allison AC. Protection afforded by sickle-cell trait against subtertian malarial infection. BMJ. 1954;1:290–4.
Bender M, Douthitt Seibel G. Sickle cell disease. 1993. https://www.ncbi.nlm.nih.gov/books/NBK1377/.
Ohene-Frempong K, Weiner SJ, Sleeper LA, et al. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood. 1998;91:288–94.
Gemmete JJ, Davagnanam I, Toma AK, et al. Arterial ischemic stroke in children. Neuroimaging Clin N Am. 2013;23:781–98. https://doi.org/10.1016/j.nic.2013.03.019.
Strouse JJ, Jordan LC, Lanzkron S, Casella JF. The excess burden of stroke in hospitalized adults with sickle cell disease. Am J Hematol. 2009;84:548–52. https://doi.org/10.1002/ajh.21476.
Kirkham FJ. Therapy Insight: stroke risk and its management in patients with sickle cell disease. Nat Clin Pract Neurol. 2007;3:264–78. https://doi.org/10.1038/ncpneuro0495.
Lawrence C, Webb J. Sickle cell disease and stroke: diagnosis and management. Curr Neurol Neurosci Rep. 2016;16:27. https://doi.org/10.1007/s11910-016-0622-0.
Schnog JB, Mac Gillavry MR, van Zanten AP, et al. Protein C and S and inflammation in sickle cell disease. Am J Hematol. 2004;76:26–32. https://doi.org/10.1002/ajh.20052.
Yasin Z, Witting S, Palascak MB, et al. Phosphatidylserine externalization in sickle red blood cells: associations with cell age, density, and hemoglobin F. Blood. 2003;102:365–70. https://doi.org/10.1182/blood-2002-11-3416.
Switzer JA, Hess DC, Nichols FT, Adams RJ. Pathophysiology and treatment of stroke in sickle-cell disease: present and future. Lancet Neurol. 2006;5:501–12. https://doi.org/10.1016/S1474-4422(06)70469-0.
Francis RB, Haywood LJ. Elevated immunoreactive tumor necrosis factor and interleukin-1 in sickle cell disease. J Natl Med Assoc. 1992;84:611–5.
Hines PC, McKnight TP, Seto W, et al. Central nervous system events in children with sickle cell disease presenting acutely with headache. J Pediatr. 2011;159:472–8. https://doi.org/10.1016/j.jpeds.2011.02.009.
Seeler RA, Royal JE, Powe L, Goldberg HR. Moyamoya in children with sickle cell anemia and cerebrovascular occlusion. J Pediatr. 1978;93:808–10.
Powars D, Adams RJ, Nichols FT, et al. Delayed intracranial hemorrhage following cerebral infarction in sickle cell anemia. J Assoc Acad Minor Phys. 1990;1:79–82.
Powars D, Wilson B, Imbus C, et al. The natural history of stroke in sickle cell disease. Am J Med. 1978;65:461–71.
Oyesiku NM, Barrow DL, Eckman JR, et al. Intracranial aneurysms in sickle-cell anemia: clinical features and pathogenesis. J Neurosurg. 1991;75:356–63. https://doi.org/10.3171/jns.1991.75.3.0356.
Armstrong FD, Thompson RJ, Wang W, et al. Cognitive functioning and brain magnetic resonance imaging in children with sickle Cell disease. Neuropsychology Committee of the Cooperative Study of Sickle Cell Disease. Pediatrics. 1996;97:864–70.
Miller ST, Macklin EA, Pegelow CH, et al. Silent infarction as a risk factor for overt stroke in children with sickle cell anemia: a report from the cooperative study of sickle cell disease. J Pediatr. 2001;139:385–90. https://doi.org/10.1067/mpd.2001.117580.
Adams R, McKie V, Nichols F, et al. The use of transcranial ultrasonography to predict stroke in sickle cell disease. N Engl J Med. 1992;326:605–10. https://doi.org/10.1056/NEJM199202273260905.
Driscoll MC, Hurlet A, Styles L, et al. Stroke risk in siblings with sickle cell anemia. Blood. 2003;101:2401–4.
Sampaio Silva G, Vicari P, Figueiredo MS, et al. Transcranial doppler in adult patients with sickle cell disease. Cerebrovasc Dis. 2006;21:38–41. https://doi.org/10.1159/000089592.
Flanagan JM, Frohlich DM, Howard TA, et al. Genetic predictors for stroke in children with sickle cell anemia. Blood. 2011;117:6681–4. https://doi.org/10.1182/blood-2011-01-332205.
Lettre G, Sankaran VG, Bezerra MAC, et al. DNA polymorphisms at the BCL11A, HBS1L-MYB, and -globin loci associate with fetal hemoglobin levels and pain crises in sickle cell disease. Proc Natl Acad Sci. 2008;105:11869–74. https://doi.org/10.1073/pnas.0804799105.
Hoppe C, Klitz W, Cheng S, et al. Gene interactions and stroke risk in children with sickle cell anemia. Blood. 2004;103:2391–6. https://doi.org/10.1182/blood-2003-09-3015.
Sebastiani P, Ramoni MF, Nolan V, et al. Genetic dissection and prognostic modeling of overt stroke in sickle cell anemia. Nat Genet. 2005;37:435–40. https://doi.org/10.1038/ng1533.
JGT VI, Tang DC, Savage SA, et al. Variants in the VCAM1 gene and risk for symptomatic stroke in sickle cell disease. Blood. 2002;100:4303–9. https://doi.org/10.1182/blood-2001-12-0306.
Hoppe C, Klitz W, Noble J, et al. Distinct HLA associations by stroke subtype in children with sickle cell anemia. Blood. 2003;101:2865–9. https://doi.org/10.1182/blood-2002-09-2791.
Flanagan JM, Sheehan V, Linder H, et al. Genetic mapping and exome sequencing identify 2 mutations associated with stroke protection in pediatric patients with sickle cell anemia. Blood. 2013;121:3237–45. https://doi.org/10.1182/blood-2012-10-464156.
Geard A, Pule GD, Chelo D, et al. Genetics of sickle cell-associated cardiovascular disease: an expert review with lessons learned in Africa. Omi A J Integr Biol. 2016;20:581–92. https://doi.org/10.1089/omi.2016.0125.
Johnson CS. Arterial blood pressure and hyperviscosity in sickle cell disease. Hematol Oncol Clin North Am. 2005;19:827–37. https://doi.org/10.1016/j.hoc.2005.08.006.
Estcourt LJ, Fortin PM, Hopewell S, et al. Blood transfusion for preventing primary and secondary stroke in people with sickle cell disease. Cochrane Database Syst Rev. 2017;11:CD003146.
Adams RJ, McKie VC, Hsu L, et al. Prevention of a first stroke by transfusions in children with sickle cell anemia and abnormal results on transcranial doppler ultrasonography. N Engl J Med. 1998;339:5–11. https://doi.org/10.1056/NEJM199807023390102.
Investigators TOPSP in SCA (STOP 2) T. Discontinuing prophylactic transfusions used to prevent stroke in sickle cell disease. N Engl J Med. 2005;353:2769–78. https://doi.org/10.1056/NEJMoa050460.
Razvi SSM, Davidson R, Bone I, Muir KW. The prevalence of cerebral autosomal dominant arteriopathy with subcortical infarcts and leucoencephalopathy (CADASIL) in the west of Scotland. J Neurol Neurosurg Psychiatry. 2005;76:739–41. https://doi.org/10.1136/jnnp.2004.051847.
Narayan SK, Gorman G, Kalaria RN, et al. The minimum prevalence of CADASIL in northeast England. Neurology. 2012;78:1025–7. https://doi.org/10.1212/WNL.0b013e31824d586c.
Kilarski LL, Rutten-Jacobs LCA, Bevan S, et al. Prevalence of CADASIL and Fabry disease in a Cohort of MRI defined younger onset lacunar stroke. PLoS One. 2015;10:e0136352. https://doi.org/10.1371/journal.pone.0136352.
Tan RYY, Markus HS. CADASIL: Migraine, Encephalopathy, Stroke and Their Inter-Relationships. PLoS One. 2016;11:e0157613. https://doi.org/10.1371/journal.pone.0157613.
Adib-Samii P, Brice G, Martin RJ, Markus HS. Clinical spectrum of CADASIL and the effect of cardiovascular risk factors on phenotype: study in 200 consecutively recruited individuals. Stroke. 2010;41(4):630. https://doi.org/10.1161/STROKEAHA.109.568402.
Joutel A, Vahedi K, Corpechot C, et al. Strong clustering and stereotyped nature of Notch3 mutations in CADASIL patients. Lancet. 1997;350:1511–5. https://doi.org/10.1016/S0140-6736(97)08083-5.
Singhal S, Bevan S, Barrick T, et al. The influence of genetic and cardiovascular risk factors on the CADASIL phenotype. Brain. 2004;127:2031–8. https://doi.org/10.1093/brain/awh223.
Opherk C, Peters N, Holtmannspötter M, et al. Heritability of MRI lesion volume in CADASIL: evidence for genetic modifiers. Stroke. 2006;37:2684–9. https://doi.org/10.1161/01.STR.0000245084.35575.66.
Peters N, Holtmannspotter M, Opherk C, et al. Brain volume changes in CADASIL: a serial MRI study in pure subcortical ischemic vascular disease. Neurology. 2006;66:1517–22. https://doi.org/10.1212/01.wnl.0000216271.96364.50.
Singhal S, Rich P, Markus HS. The spatial distribution of MR imaging abnormalities in cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy and their relationship to age and clinical features. AJNR Am J Neuroradiol. 2005;26:2481–7.
Investigators TS. Effects of clopidogrel added to aspirin in patients with recent lacunar stroke. N Engl J Med. 2012;367:817–25. https://doi.org/10.1056/NEJMoa1204133.
Donnini I, Nannucci S, Valenti R, et al. Acetazolamide for the prophylaxis of migraine in CADASIL: a preliminary experience. J Headache Pain. 2012;13:299–302. https://doi.org/10.1007/s10194-012-0426-9.
Forteza AM, Brozman B, Rabinstein AA, et al. Acetazolamide for the treatment of migraine with aura in CADASIL. Neurology. 2001;57:2144–5. https://doi.org/10.1212/WNL.57.11.2144.
Weller M, Dichgans J, Klockgether T. Acetazolamide-responsive migraine in CADASIL. Neurology. 1998;50:1505. https://doi.org/10.1212/WNL.50.5.1505.
Martikainen MH, Roine S. Rapid improvement of a complex migrainous episode with sodium valproate in a patient with CADASIL. J Headache Pain. 2012;13:95–7. https://doi.org/10.1007/s10194-011-0400-y.
MHRA. Imigran 100 mg tablets (sumatriptan succinate) patient information leaflet. In: Medical information and production details. 2013. http://www.medicines.org.uk/emc/medicine/749. Accessed 27 Sept 2015.
Schon F, Martin RJ, Prevett M, et al. “CADASIL coma”: an underdiagnosed acute encephalopathy. J Neurol Neurosurg Psychiatry. 2003;74:249–52. https://doi.org/10.1136/jnnp.74.2.249.
Zheng DM, FF X, Gao Y, et al. A Chinese pedigree of cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy (CARASIL): clinical and radiological features. J Clin Neurosci. 2009;16:847–9. https://doi.org/10.1016/j.jocn.2008.08.031.
Mendioroz M, Fernández-Cadenas I, Del Río-Espinola A, et al. A missense HTRA1 mutation expands CARASIL syndrome to the Caucasian population. Neurology. 2010;75:2033–5. https://doi.org/10.1212/WNL.0b013e3181ff96ac.
Nozaki H, Sekine Y, Fukutake T, et al. Characteristic features and progression of abnormalities on MRI for CARASIL. Neurology. 2015;85:459–63. https://doi.org/10.1212/WNL.0000000000001803.
Yanagawa S, Ito N, Arima K, Ikeda S -i S. Cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy. Neurology. 2002;58:817–20. https://doi.org/10.1212/WNL.58.5.817.
Oka C, Tsujimoto R, Kajikawa M, et al. HtrA1 serine protease inhibits signaling mediated by Tgfbeta family proteins. Development. 2004;131:1041–53. https://doi.org/10.1242/dev.00999.
Chen Y, He Z, Meng S, et al. A novel mutation of the high-temperature requirement A serine peptidase 1 (HTRA1) gene in a Chinese family with cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy (CARASIL). J Int Med Res. 2013;41:1445–55. https://doi.org/10.1177/0300060513480926.
Gunda B, Mine M, Kovács T, et al. COL4A2 mutation causing adult onset recurrent intracerebral hemorrhage and leukoencephalopathy. J Neurol. 2014;261(3):500. https://doi.org/10.1007/s00415-013-7224-4.
Breedveld G, de Coo IF, Lequin MH, et al. Novel mutations in three families confirm a major role of COL4A1 in hereditary porencephaly. J Med Genet. 2006;43:490–5. https://doi.org/10.1136/jmg.2005.035584.
Alamowitch S, Plaisier E, Favrole P, et al. Cerebrovascular disease related to COL4A1 mutations in HANAC syndrome. Neurology. 2009;73:1873–82. https://doi.org/10.1212/WNL.0b013e3181c3fd12.
Jeanne M, Labelle-Dumais C, Jorgensen J, et al. COL4A2 mutations impair COL4A1 and COL4A2 secretion and cause hemorrhagic stroke. Am J Hum Genet. 2012;90:91–101. https://doi.org/10.1016/j.ajhg.2011.11.022.
Plaisier E, Gribouval O, Alamowitch S, et al. COL4A1 mutations and hereditary angiopathy, nephropathy, aneurysms, and muscle cramps. N Engl J Med. 2007;357:2687–95. https://doi.org/10.1056/NEJMoa071906.
Rannikmäe K, Davies G, Thomson PA, et al. Common variation in COL4A1/COL4A2 is associated with sporadic cerebral small vessel disease. Neurology. 2015;84(9):918–26. https://doi.org/10.1212/WNL.0000000000001309.
Linn J, Halpin A, Demaerel P, et al. Prevalence of superficial siderosis in patients with cerebral amyloid angiopathy. Neurology. 2010;74:1346–50. https://doi.org/10.1212/WNL.0b013e3181dad605.
Vinters HV. Cerebral amyloid angiopathy. A critical review. Stroke. 1987;18:311–24.
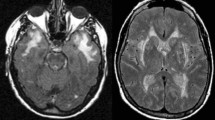
Thanprasertsuk S, Martinez-Ramirez S, Pontes-Neto OM, et al. Posterior white matter disease distribution as a predictor of amyloid angiopathy. Neurology. 2014;83:794–800. https://doi.org/10.1212/WNL.0000000000000732.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Tan, R.Y.Y., Markus, H.S. (2018). Genetics and Genomics of Stroke. In: Kumar, D., Elliott, P. (eds) Cardiovascular Genetics and Genomics. Springer, Cham. https://doi.org/10.1007/978-3-319-66114-8_24
Download citation
DOI: https://doi.org/10.1007/978-3-319-66114-8_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-66112-4
Online ISBN: 978-3-319-66114-8
eBook Packages: MedicineMedicine (R0)