Abstract
Glial tumors are primary tumors of the central nervous system and can be divided into low and high-grade tumors. Even though there are no randomized control studies on extent of resection, there is a growing body of evidence supporting maximal, safe resection when surgery is pursued for patients with these tumors. The management of low-grade gliomas (World Health Organization grade II tumors) consists of maximal surgical resection without causing deficits for tumors that are growing or causing mass effect. Incidentally discovered, small low-grade gliomas can be considered for routine surveillance with frequent imaging. High-grade gliomas (World Health Organization grade III and IV tumors) should undergo maximal surgical resection while avoiding iatrogenic deficits. Despite maximal surgical resection, the majority of patients with both low and high-grade tumors will inevitably have recurrence and eventually die from progressive disease. The majority of this recurrence occurs in close proximity to the tumor margins. One type of adjuvant therapy that has been developed to increase radiation to the tumor margins while minimizing toxicity to surrounding normal brain parenchyma is intra-cavitary radiopharmaceutical therapy, also known as brachytherapy. This therapy involves placement of radioisotopes in the tumor bed either peri- or postoperatively and shows promise in that patients with both low and grade gliomas can undergo local radiation therapy, and therefore are not subjected to the neurocognitive problems associated with external brain radiation and the systemic toxicity of chemotherapy. However, clinical trials have yet to show a significant survival benefit for patients undergoing brachytherapy.
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Gliomas are primary tumors of the central nervous system that can be subdivided into low- and high-grade gliomas. Patients with low-grade gliomas are considered to have a better prognosis than patients harboring high-grade tumors [1–13]. The median survival for patients with low-grade gliomas is between 5 and 10 years as compared to 1–3 years for patients with high-grade tumors [1–13]. Regardless of tumor grade, the overwhelming majority of patients will eventually die from progressive and/or recurrent disease [1–13]. Despite the poor prognosis for patients with gliomas, surgery has been a mainstay of treatment [1–13]. An emerging adjunct to surgical therapy is stereotactic brachytherapy (SBT) [14, 15]. This chapter will discuss the role that surgery and brachytherapy have for patients with gliomas.
Role of Surgery for Patients with High-Grade Gliomas
High-grade gliomas include WHO grade III (anaplastic astrocytomas) and IV (glioblastoma—GB). Patients with high-grade gliomas are considered to have poor prognoses [3–6, 12, 13, 16–19]. Patients with anaplastic tumors have a median survival of approximately 3 years, while patients with GB have a median survival of approximately 14 months [2–6, 10, 11, 18–20]. High-grade gliomas are characterized by their invasive and infiltrative nature, making curative resection unlikely [20]. In fact, survival has changed little in recent years despite advances in medical and surgical therapies [21]. Walter Dandy in the 1920s performed hemispherectomies for these lesions, and they would still recur on the contralateral side [22]. Survival for these patients was still less than 2 years [22]. As a result, the efficacy of surgery alone for these lesions has been questioned and raises the need to implement further treatment modalities to complement surgery.
In recent years, there have been an increased number of studies supporting a role for extensive surgery in patients with high-grade gliomas.
Lacroix et al. in 2001 analyzed 416 consecutive patients with GBM [23]. They found that resections greater than 98 % were needed to significantly improve survival, where survival increased from 8.8 to 13 months [23]. This study, however, did not include adjuvant therapy into their survival analysis [23]. Sanai et al. more recently studied 500 patients with GB in 2011 and found that 78 % resection was needed to confer a survival advantage [24]. Keles et al. in 2006 evaluated 102 patients with anaplastic astrocytomas [25]. They found that the amount of residual tumor correlated with time to progression and overall survival, where the most significant threshold was 10 cm3 [25]. This study, however, did not include patients with GB and did not account for extent of resection, just residual disease [25]. Laws and colleagues evaluated outcomes for 788 patients with malignant astrocytomas from several institutions [26]. They found that patients who underwent surgical resection had significantly longer survival times than patients who underwent biopsy [26]. This remained significant even after eliminating patients who were considered poor surgical candidates [26]. This study, however, did not evaluate the role of gross total, near total, or subtotal resection [26].
We recently evaluated the role of extent of resection on survival for 949 patients with malignant astrocytomas [12]. We found that there was a survival benefit for patients who underwent both gross total and near total resection [12]. This survival benefit was independent of age, degree of disability, or subsequent treatment modalities for both WHO grade III and IV gliomas [12]. The median survival for patients with newly diagnosed GB who underwent gross total, near total, and subtotal resection was 13, 11, and 8 months, respectively [12]. Likewise, the median survival for patients with recurrent GB who underwent gross total, near total, and subtotal resection was 11, 9, and 5 months, respectively [12]. Similarly, for patients with WHO grade III astrocytomas, patients who underwent gross total resection had improved survival as compared to patients with subtotal resection, even after controlling for age, functional status, and revision resection [12]. The median survival after primary resection of WHO III astrocytomas for gross total, near total, and subtotal resection was 58, 46, and 34 months, respectively [12]. These studies therefore suggest that achieving an increased extent of resection may be associated with prolonging survival for patients with malignant astrocytomas, but randomized control studies do not exist.
Despite this growing body of evidence supporting increased extent of resection for patients with high-grade gliomas, not all studies support a positive correlation between extent of resection and survival [27]. Levin et al. studied 90 patients with WHO grade III gliomas enrolled into a phase II study for radiation and carboplatin [27]. They found that extent of resection was not significantly associated with survival for this cohort [27]. Totrosa et al. also found no association between survival and extent of resection for a similar group of patients with anaplastic tumors [28]. Additionally, Pope et al. evaluated 153 patients with high-grade gliomas (43 with WHO grade III and 110 with WHO grade IV gliomas) [29]. They found no difference in survival between patients who underwent surgery versus biopsy [29].
There have been five systematic reviews of the literature to date evaluating the role of resection and survival [30–34]. Sanai and colleagues identified 28 studies on high-grade gliomas with more than 75 patients [34]. They found of these 28 studies, 14 studies demonstrated an association between extent of resection and survival and ten studies found no statistical association [34]. Grant et al. performed a Cochrane review on biopsy versus resection for patients with high-grade gliomas [30]. They excluded all 2,100 identified studies because they lacked statistical power, patient information, and/or outcome data [30]. Hess [31] and Nazzaro [32] also independently performed similar reviews and also concluded that there was a lack of high-quality studies to conclude if surgical resection provided a benefit for patients with high-grade gliomas [31].
Although the survival benefit of extensive surgical resection is not demonstrated in all retrospective studies, the prevailing consensus in numerous studies have demonstrated that gross total resection of gliomas improves overall survival in comparison to subtotal resection and biopsy [2–6, 10, 11, 30–32]. In addition to the possible benefit of prolonging survival with safe, maximal surgical debulking, aggressive resection provides a more representative sample for pathological diagnosis and may also provide more improvement in mass effect with subsequent symptomatic relief [26]. Maximal resection should therefore be pursued when safe to do so for high-grade lesions (Table 18.1) [19].
Role of Surgery for Patients with Low-Grade Gliomas
Patients with low-grade gliomas often have a better prognosis than patients harboring higher-grade tumors [3–10, 12, 18–21]. In fact, the median survival for patients with low-grade gliomas is typically between 5 and 10 years [3–10, 12, 18–21]. Despite this more favorable prognosis, 50–75 % of patients with low-grade gliomas eventually die from their disease because of either tumor progression or degeneration to a higher malignant grade [1, 7, 8]. The optimal treatment for patients who harbor low-grade gliomas, however, remains unclear because many patients are followed radiographically and intervention is only pursued when clinical or radiographic progression becomes evident [35]. Moreover, the role of surgery in delaying recurrence and/or malignant degeneration as well as prolonging survival remains controversial [7, 35].
This lack of understanding of the effectiveness of surgery for patients with low-grade gliomas is because there are no randomized control trials or matched pair analyses. Keles et al. performed a literature review of the role of surgery for patients with low-grade gliomas and found 30 studies evaluating the role of surgery for patients with low-grade gliomas [1]. In this review, all but five studies were excluded because they included patients with grade I gliomas, relied upon intraoperative determination of extent of resection, and had small sample sizes, among others [36–39]. These five studies that met the inclusion criteria were also limited because extent of resection was determined by intraoperative gross visualization rather than neuro-imaging, and a distinction between gross total and near total resection was not made [36–39]. This review and others have found data supporting a role of surgery in delaying recurrence and prolonging survival controversial [1, 40].
Despite this, there are an increasing number of studies demonstrating a benefit for increasing extent of resection for patients with low-grade gliomas [7]. Wisoff et al. evaluated 518 pediatric patients with low-grade glioma, and found that extent of resection was significantly associated with improved progression-free survival [41]. The 5-year survival rate was 99 % with gross total resection, 95 % with 1.5 cm3 residual disease, 94 % with 1.5–2.9 cm3 residual, and 87 % with >3 cm3 residual [41]. The 5-year progression-free survival rate was 90 % with gross total resection and 45–65 % with any volume (1.5–3 cm3) of residual disease [41]. More recently, Smith et al. performed a retrospective volumetric analysis of extent of hemispheric LGG resection in 216 patients and found that patients with at least 90 % resection had 5- and 8-year survival rates of 97 % and 91 %, respectively, while patients with less than 90 % resection had 5- and 8-year survival rates of 76 % and 60 %, respectively [42]. We recently evaluated 170 patients with low-grade gliomas and found that gross-total resection was associated with increased overall survival as compared to patients who underwent subtotal resection [11]. Five-year overall survival after gross total, near total, and subtotal resection was 95 %, 80 %, 70 %, respectively, and 10-year survival was 76 %, 57 %, and 49 %, respectively [11]. Additionally, after gross total, near total, and subtotal resection, median time to tumor progression was 7.0, 4.0, and 3.5 years, respectively [11]. The median time to malignant degeneration after gross total, near total, and subtotal resection was 12.5, 5.8, and 7 years, respectively [11]. In a separate study, we found that gross total resection was independently associated with delayed malignant degeneration [7].
There is a growing body of evidence that surgery is an effective treatment for patients with low-grade gliomas, despite an absence of randomized control trials. For patients who present with large tumors, significant neurological deficits, and medically intractable seizures, immediate surgical intervention is generally the preferred treatment option [7, 43]. Extensive resection without causing an iatrogenic deficit can lead to improvements in overall survival, progression-free survival, and malignant transformation-free survival [7–9, 44]. However, for incidentally discovered small tumors without mass effect or symptoms, observation with surveillance imaging is a viable option given the slow growth and natural history of low-grade gliomas (Table 18.1) [45].
Intra-Cavitary Radiopharmaceutical Therapy or Stereotactic Brachytherapy
The standard of care for patients with high-grade gliomas is extensive resection, followed by radiation and temozolomide chemotherapy [46]. Regardless of treatment, tumor recurrence typically occurs close to the tumor margins [20]. At the tumor margin, there is an increased tumor cell density [20]. Beyond the periphery, there is a sharp fall-off in cell numbers as the distance from the resection cavity increases [20]. Extensive surgical resection of gliomas can prolong progression-free and overall survival by decreasing tumor burden and possibly increasing adjuvant therapy efficacy as it has with other types of solid tumors [47]. Moreover, the use of adjuvant therapies have been developed to help reduce the tumor burden at the tumor periphery. One of these developments is SBT (Table 18.2).
It is generally considered beneficial to provide radiation to the gliomatous areas around the surgical cavity, especially for high-grade gliomas [14, 48, 49]. The techniques to deliver this radiation include stereotactic radiation therapy and SBT [14, 48, 49]. SBT involves the delivery of radiation by stereotactically implanting radioactive sources near or within tumors [14, 48, 49]. SBT can be applied peri- or postoperatively by either permanent isotope seeds or by temporary catheters containing radioisotopes [14, 48, 49]. There are a variety of different isotopes that can be administered for radiation therapy including Iodine-125, Iodine-131, and Iridium-192, among others [14, 48, 49]. The exposure times of these seeds range from a few days to several months and vary whether temporary implants or permanent seeds are used [14, 48, 49]. In the central nervous system, the most common radioactive source used for SBT are Iodine-125 seeds (125I) which emit low-energy radiation of 0.028–0.035 meV and have a steep falloff dose that reduces peripheral normal tissue exposure [14, 15].
SBT has been used as adjuvant treatment following surgical resection for both primary and recurrent low- and high-grade gliomas and has been used for tumors in eloquent regions that are considered unresectable [14, 48, 49]. The theoretical benefit of SBT is that it allows for precise surgical implantation of radioisotopes within the tumor or tumor cavity, thus providing local radiation to adjacent tissue while sparing surrounding tissue [15]. Additionally, SBT avoids the systemic side effects of chemotherapy and the potential neuro-cognitive effects of external beam radiation therapy (EBRT) [50]. However, while numerous retrospective studies have demonstrated SBT to be safe and efficacious in gliomas [15, 51–56], three small single institution prospective randomized trials failed to demonstrate a survival advantage [57–59]. Therefore, the efficacy of this treatment option requires further investigation as well as potential advances in imaging and implant technology before it will be widely used.
Procedure
SBT is based on the principle that radiation will induce necrosis in a targeted tumor volume and that necrotic tissue will then be removed by macrophages [60]. Stereotactic computed tomography and magnetic resonance images (MRI) are co-registered for treatment planning and dosimetry calculations [61]. The typical cumulative, prescribed dose ranges from 50–65 Gy over 3–5 days [14, 48, 49]. In interstitial radiotherapy, 125I seeds are administered via stereotactically implanted catheters intraoperatively [15, 62]. Dose rates vary and individual institutions vary over whether a low dose, which allows build up of damage in tumor cells, or a high dose rate, which decreases total treatment time, is administered [14]. A potential barrier to the success of radioactive seed brachytherapy may be the inhomogeneous distribution of doses [14, 48, 49]. Tumor areas adjacent to seeds receive a very high dose that may contribute to toxicity, whereas the areas in between seeds may have cold spots and the tumor is potentially under-dosed in these regions [63].
Recently, the advent of GliaSite brachytherapy allows for administration of 125I on an outpatient basis [64–66]. With GliaSite, an expandable balloon catheter can be implanted intracranially near the tumor or within a resection cavity thereby providing a conformal fit (Fig. 18.1) [64–66]. Liquid 125I is then used as the source of radiation and the balloon is inflated through an accessible subcutaneous port; this administration provides the opportunity for treatment to be administered after several weeks of postoperative recovery [66, 67]. As the liquid radioisotope distributes uniformly throughout the balloon, there is a uniform delivery of radiation to the region surrounding the balloon [64–66]. This minimizes the potential for “hot” or “cold” radiation regions and also allows for a predictable distribution of radiation dose, which decreases with distance from the balloon surface [64–66]. Whereas stereotactic implantation of radiation seed catheters can be placed in the midst of actual gross tumor, the GliaSite technique is only useful when a surgical cavity has been created by resection of all or most of the tumor [64–66]. There also continues to be interest in developing targeted delivery of radiation dose by using radioisotopes bound to molecules, which preferentially bind to glioma cells [64–66]. In addition to 125I, I-131 labeled TM-601, a synthetic chlorotoxin, has also been demonstrated to effectively deliver radiation [68]. Efficacy has not been demonstrated, but this general approach remains promising and continues to be a subject of investigation.
Indications
Therapeutic management of gliomas includes some combination of stereotactic biopsy and radiologic monitoring, surgical resection, and chemo-radiation therapy [3–5, 16]. Although surgical resection is the gold standard, tumors located in eloquent or critical areas of the brain are not always amenable to extensive debulking [49]. In children with inoperable low-grade gliomas, SBT is a treatment option that avoids the hematologic and otologic toxicity of chemotherapy and the cognitive and neuropsychological deficits associated with EBRT [50, 69]. In these children, retrospective studies have found SBT to be safe and have an efficacy that is comparable to conventional chemo-radiation with 5 and 10-year survival rates of 97 % and 92 %, respectively [51, 52, 69]. Additionally, in adults with low-grade gliomas, the combination of SBT and microsurgery reduces the high complication rate of injury to eloquent brain regions while effectively irradiating the tumor in several retrospective studies [56, 70, 71]. For high-grade gliomas, SBT has been utilized for both operated and inoperable gliomas in combination with adjuvant therapies and has been shown to be safely tolerated [55, 72]. Several studies have retrospectively studied the safety and feasibility of SBT in high-grade gliomas using GliaSite in combination with resected brain tumors [66, 67].
Previous Studies
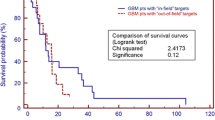
Previous studies (Table 18.3) have demonstrated the safety and efficacy of brachytherapy for patients with gliomas. Gutin et al. studied 63 patients who were administered brachytherapy (125I) in addition to EBRT, procarbazine, lomustine, and vincristine from 1982 to 1990. The median survival for patients with anaplastic gliomas was 157 weeks for those with implants and 165 weeks for those without implants, while the median survival for patients with GB was 88 weeks for those with implants and 67 weeks for those without implants [73]. Wen and colleagues treated 56 patients with GB from 1987 to 1993 [74]. The patients in this study underwent surgery, limited field EBRT, and brachytherapy with 125I [74]. The median survival for patients undergoing brachytherapy was 18 months compared with 11 months for a matched brachytherapy control group with similar clinical and radiologic features [74]. Thirty six patients (64 %), however, underwent reoperation for symptomatic radiation necrosis [74]. Welsh et al. studied 20 patients from eight institutions who underwent Gliasite brachytherapy boost [66]. These patients underwent extensive debulking followed by EBRT [66]. The average survival for this study population was 11.4 months, which was 3 months longer than historical controls [66]. Three patients (14 %) in this series experienced central nervous system toxicity [66].
In addition to these studies, there have been two randomized control studies to date on the use of brachytherapy for patients with gliomas (Table 18.3) [58, 59]. Selker and colleagues randomized 270 patients with newly diagnosed malignant gliomas to surgery, EBRT, and carmustine or surgery, EBRT, carmustine, and interstitial radiotherapy boost with 125I from 1987 to 1994 [59]. The median survival for patients undergoing treatment with 125I was 68.1 weeks as compared to 58.8 weeks [59]. The difference in survival was not statistically significant [59]. Likewise, Laperriere et al. randomized 140 patients from 1986 to 1996 to brachytherapy (125I) plus EBRT versus EBRT for patients with biopsy-proven malignant astrocytomas [58]. The 71 patients randomized to the implant arm had a median survival of 13.8 months as compared to 13.2 months for the 69 patients with EBRT [58]. There was no significant difference in survival between the two treatment arms [58]. Thus, while SBT remains a treatment option for both low- and high-grade gliomas, the data is conflicting and inconclusive. This is true when SBT is used in combination with standard surgical resection and/or chemo-radiation.
Limitations and Complications
The risks and benefits of SBT are summarized in Table 18.2. Patients who are more amenable to SBT include those with tumors that are smaller <5 cm in diameter to minimize damage to surrounding brain parenchyma [62]. Moreover, patient selection is limited to those with spherical tumors, as ovoid or complex polycyclic shapes create challenges in obtaining uniform dose distributions [62, 70]. Complications that are due to SBT radiation most commonly lead to blood-brain barrier breakdown at high radiation doses and result in radiation-induced necrosis [75]. Necrotizing radiation changes can cause mass effect and lead to devastating side effects including both transient and long-term neurological dysfunction, increased use of steroids to reduce edema, and formation of cysts that can exert mass effect [62, 70].
The GliaSite balloon brachytherapy is designed for surgical cavities up to 3–4 cm in size [64–66]. A substantial radiation dose can be delivered up to a cm or more beyond the balloon surface such that minimal gross residual disease can be encompassed [64–66]. However, the higher doses required to deliver a sufficient amount of radiation at increasing distances from the balloon surface may result in more toxicity [64–66]. More study of this technique are therefore required.
Conclusion
While there are no randomized control trials, there is a growing body of evidence supporting maximal resection without causing an iatrogenic deficit for patients with high-grade gliomas, as well as low-grade glioma patients with symptoms or enlarging tumors. SBT can be utilized as adjuvant treatment for primary and recurrent low- and high-grade gliomas in combination with surgical resection, chemotherapy, and/or EBRT. The use of intracranial SBT can also be helpful for patients with tumors located in functionally critical areas not amenable to surgical resection. However, to date, randomized control trials have yet to show a survival benefit for patients with SBT. Thus, while SBT can be utilized in a select group of patients to minimize adverse side effects of surgical and chemo-radiation treatment, more evidence is needed to determine whether patient outcomes are significantly improved with this therapy. The development of new approaches or new radiopharmaceutical agents to deliver intra-cavitary brachytherapy such as the GliaSite balloon catheter which delivers a predictable homogeneous dose distribution or the use of radiolabelled antibodies to target treatment at tumor cells has the potential to enhance the therapeutic ratio of this approach.
References
Keles GE, Lamborn KR, Berger MS. Low-grade hemispheric gliomas in adults: a critical review of extent of resection as a factor influencing outcome. J Neurosurg. 2001;95(5):735–45.
Piepmeier J, Baehring JM. Surgical resection for patients with benign primary brain tumors and low grade gliomas. J Neurooncol. 2004;69(1–3):55–65.
Chaichana KL, Chaichana KK, Olivi A, Weingart JD, Bennett R, Brem H, et al. Surgical outcomes for older patients with glioblastoma multiforme: preoperative factors associated with decreased survival. J Neurosurg. 2011;114(3):587–94. Clinical article.
Chaichana K, Parker S, Olivi A, Quinones-Hinojosa A. A proposed classification system that projects outcomes based on preoperative variables for adult patients with glioblastoma multiforme. J Neurosurg. 2010;112(5):997–1004 [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t].
Chaichana KL, Garzon-Muvdi T, Parker S, Weingart JD, Olivi A, Bennett R, et al. Supratentorial glioblastoma multiforme: the role of surgical resection versus biopsy among older patients. Ann Surg Oncol. 2011;18(1):239–45 [Clinical Trial].
Chaichana KL, Kosztowski T, Niranjan A, Olivi A, Weingart JD, Laterra J, et al. Prognostic significance of contrast-enhancing anaplastic astrocytomas in adults. J Neurosurg. 2010;113(2):286–92 [Research Support, Non-U.S. Gov’t].
Chaichana KL, McGirt MJ, Laterra J, Olivi A, Quinones-Hinojosa A. Recurrence and malignant degeneration after resection of adult hemispheric low-grade gliomas. J Neurosurg. 2010;112(1):10–7.
Chaichana KL, McGirt MJ, Niranjan A, Olivi A, Burger PC, Quinones-Hinojosa A. Prognostic significance of contrast-enhancing low-grade gliomas in adults and a review of the literature. Neurol Res. 2009;31(9):931–9.
Chaichana KL, McGirt MJ, Woodworth GF, Datoo G, Tamargo RJ, Weingart J, et al. Persistent outpatient hyperglycemia is independently associated with survival, recurrence and malignant degeneration following surgery for hemispheric low grade gliomas. Neurol Res. 2010;32(4):442–8.
Chaichana KL, Zaidi H, Pendleton C, McGirt MJ, Grossman R, Weingart JD, et al. The efficacy of carmustine wafers for older patients with glioblastoma multiforme: prolonging survival. Neurol Res. 2011;33(7):759–64.
McGirt MJ, Chaichana KL, Attenello FJ, Weingart JD, Than K, Burger PC, et al. Extent of surgical resection is independently associated with survival in patients with hemispheric infiltrating low-grade gliomas. Neurosurgery. 2008;63(4):700–7; author reply 7–8.
McGirt MJ, Chaichana KL, Gathinji M, Attenello FJ, Than K, Olivi A, et al. Independent association of extent of resection with survival in patients with malignant brain astrocytoma. J Neurosurg. 2009;110(1):156–62.
McGirt MJ, Than KD, Weingart JD, Chaichana KL, Attenello FJ, Olivi A, et al. Gliadel (BCNU) wafer plus concomitant temozolomide therapy after primary resection of glioblastoma multiforme. J Neurosurg. 2009;110(3):583–8 [Comparative Study].
Liu BL, Cheng JX, Zhang X, Zhang W. Controversies concerning the application of brachytherapy in central nervous system tumors. J Cancer Res Clin Oncol. 2010;136(2):173–85 [Review].
Ruge MI, Simon T, Suchorska B, Lehrke R, Hamisch C, Koerber F, et al. Stereotactic brachytherapy with iodine-125 seeds for the treatment of inoperable low-grade gliomas in children: long-term outcome. J Clin Oncol. 2011;29(31):4151–9.
Chaichana KL, Halthore AN, Parker SL, Olivi A, Weingart JD, Brem H, et al. Factors involved in maintaining prolonged functional independence following supratentorial glioblastoma resection. J Neurosurg. 2011;114(3):604–12. Clinical article.
Chaichana KL, Parker SL, Mukherjee D, Cheng JS, Gokaslan ZL, McGirt MJ. Assessment of the extent of surgical resection as a predictor of survival in patients with primary osseous spinal neoplasms. Clin Neurosurg. 2011;58:117–21.
Chaichana KL, Parker SL, Olivi A, Quinones-Hinojosa A. Long-term seizure outcomes in adult patients undergoing primary resection of malignant brain astrocytomas. J Neurosurg. 2009;111(2):282–92. Clinical article.
McGirt MJ, Mukherjee D, Chaichana KL, Than KD, Weingart JD, Quinones-Hinojosa A. Association of surgically acquired motor and language deficits on overall survival after resection of glioblastoma multiforme. Neurosurgery. 2009;65(3):463–9. discussion 9-70.
Quinones-Hinojosa A, Chaichana K. The human subventricular zone: a source of new cells and a potential source of brain tumors. Exp Neurol. 2007;205(2):313–24.
Tait MJ, Petrik V, Loosemore A, Bell BA, Papadopoulos MC. Survival of patients with glioblastoma multiforme has not improved between 1993 and 2004: analysis of 625 cases. Br J Neurosurg. 2007;21(5):496–500 [Randomized Controlled Trial Research Support, Non-U.S. Gov’t].
Dandy WE. Removal of right cerebral hemisphere for certain tumors with hemiplegia. JAMA. 1928;90:823–5.
Lacroix M, Abi-Said D, Fourney DR, Gokaslan ZL, Shi W, DeMonte F, et al. A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg. 2001;95(2):190–8.
Sanai N, Polley MY, McDermott MW, Parsa AT, Berger MS. An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg. 2011;115(1):3–8.
Keles GE, Chang EF, Lamborn KR, Tihan T, Chang CJ, Chang SM, et al. Volumetric extent of resection and residual contrast enhancement on initial surgery as predictors of outcome in adult patients with hemispheric anaplastic astrocytoma. J Neurosurg. 2006;105(1):34–40.
Laws ER, Parney IF, Huang W, Anderson F, Morris AM, Asher A, et al. Survival following surgery and prognostic factors for recently diagnosed malignant glioma: data from the Glioma Outcomes Project. J Neurosurg. 2003;99(3):467–73.
Levin VA, Yung WK, Bruner J, Kyritsis A, Leeds N, Gleason MJ, et al. Phase II study of accelerated fractionation radiation therapy with carboplatin followed by PCV chemotherapy for the treatment of anaplastic gliomas. Int J Radiat Oncol Biol Phys. 2002;53(1):58–66.
Tortosa A, Vinolas N, Villa S, Verger E, Gil JM, Brell M, et al. Prognostic implication of clinical, radiologic, and pathologic features in patients with anaplastic gliomas. Cancer. 2003;97(4):1063–71.
Pope WB, Sayre J, Perlina A, Villablanca JP, Mischel PS, Cloughesy TF. MR imaging correlates of survival in patients with high-grade gliomas. AJNR Am J Neuroradiol. 2005;26(10):2466–74.
Grant R, Metcalfe SE. Biopsy versus resection for malignant glioma. Cochrane Database Syst Rev. 2005;2, CD002034.
Hess KR. Extent of resection as a prognostic variable in the treatment of gliomas. J Neurooncol. 1999;42(3):227–31.
Nazzaro JM, Neuwelt EA. The role of surgery in the management of supratentorial intermediate and high-grade astrocytomas in adults. J Neurosurg. 1990;73(3):331–44.
Quigley MR, Maroon JC. The relationship between survival and the extent of the resection in patients with supratentorial malignant gliomas. Neurosurgery. 1991;29(3):385–8; discussion 8-9.
Sanai N, Berger MS. Glioma extent of resection and its impact on patient outcome. Neurosurgery. 2008;62(4):753–64; discussion 264-6.
Low-Grade Glioma Guidelines Team in association with the Guidelines and Outcomes Committee of the American Association of Neurological Surgeons. Practice parameters in adults with suspected or known supratentorial nonoptic pathway low-grade glioma. Neurosurg Focus. 1998;4(6):e10.
Philippon JH, Clemenceau SH, Fauchon FH, Foncin JF. Supratentorial low-grade astrocytomas in adults. Neurosurgery. 1993;32(4):554–9.
Rajan B, Pickuth D, Ashley S, Traish D, Monro P, Elyan S, et al. The management of histologically unverified presumed cerebral gliomas with radiotherapy. Int J Radiat Oncol Biol Phys. 1994;28(2):405–13.
van Veelen ML, Avezaat CJ, Kros JM, van Putten W, Vecht C. Supratentorial low grade astrocytoma: prognostic factors, dedifferentiation, and the issue of early versus late surgery. J Neurol Neurosurg Psychiatry. 1998;64(5):581–7.
Soffietti R, Chio A, Giordana MT, Vasario E, Schiffer D. Prognostic factors in well-differentiated cerebral astrocytomas in the adult. Neurosurgery. 1989;24(5):686–92.
Pouratian N, Schiff D. Management of low-grade glioma. Curr Neurol Neurosci Rep. 2010;10(3):224–31 [Review].
Wisoff JH, Sanford RA, Heier LA, Sposto R, Burger PC, Yates AJ, et al. Primary neurosurgery for pediatric low-grade gliomas: a prospective multi-institutional study from the Children’s Oncology Group. Neurosurgery. 2011;68(6):1548–54. [Clinical Trial Multicenter Study Research Support, N.I.H., Extramural]; discussion 54-5.
Smith JS, Chang EF, Lamborn KR, Chang SM, Prados MD, Cha S, et al. Role of extent of resection in the long-term outcome of low-grade hemispheric gliomas. J Clin Oncol. 2008;26(8):1338–45.
Sanai N, Chang S, Berger MS. Low-grade gliomas in adults. J Neurosurg. 2011;115(5):948–65 [Review].
Jung TY, Jung S, Moon JH, Kim IY, Moon KS, Jang WY. Early prognostic factors related to progression and malignant transformation of low-grade gliomas. Clin Neurol Neurosurg. 2011;113(9):752–7 [Randomized Controlled Trial].
Recht LD, Lew R, Smith TW. Suspected low-grade glioma: is deferring treatment safe? Ann Neurol. 1992;31(4):431–6.
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–96 [Clinical Trial Clinical Trial, Phase III Multicenter Study Randomized Controlled Trial Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S.].
House MG, Gonen M, Jarnagin WR, D’Angelica M, Dematteo RP, Fong Y, et al. Prognostic significance of pathologic nodal status in patients with resected pancreatic cancer. J Gastrointest Surg. 2007;11(11):1549–55.
Kreth FW, Thon N, Siefert A, Tonn JC. The place of interstitial brachytherapy and radiosurgery for low-grade gliomas. Adv Tech Stand Neurosurg. 2010;35:183–212 [Review].
Schwarz SB, Thon N, Nikolajek K, Niyazi M, Tonn JC, Belka C, et al. Iodine-125 brachytherapy for brain tumours—a review. Radiat Oncol. 2012;7:30 [Review].
Jalali R, Mallick I, Dutta D, Goswami S, Gupta T, Munshi A, et al. Factors influencing neurocognitive outcomes in young patients with benign and low-grade brain tumors treated with stereotactic conformal radiotherapy. Int J Radiat Oncol Biol Phys. 2010;77(4):974–9 [Research Support, Non-U.S. Gov’t].
Korinthenberg R, Neuburger D, Trippel M, Ostertag C, Nikkhah G. Long-term results of brachytherapy with temporary iodine-125 seeds in children with low-grade gliomas. Int J Radiat Oncol Biol Phys. 2011;79(4):1131–8.
Voges J, Sturm V, Berthold F, Pastyr O, Schlegel W, Lorenz WJ. Interstitial irradiation of cerebral gliomas in childhood by permanently implanted 125-iodine–preliminary results. Klin Padiatr. 1990;202(4):270–4.
Ostertag CB, Kreth FW. Iodine-125 interstitial irradiation for cerebral gliomas. Acta Neurochir (Wien). 1992;119(1–4):53–61.
Voges J, Sturm VV. Interstitial irradiation with stereotactically implanted I-125 seeds for the treatment of cerebral glioma. Crit Rev Neurosurg. 1999;9(4):223–33.
Voges J, Treuer H, Schlegel W, Pastyr O, Sturm V. Interstitial irradiation of cerebral gliomas with stereotactically implanted iodine-125 seeds. Acta Neurochir Suppl (Wien). 1993;58:108–11.
Kreth FW, Faist M, Grau S, Ostertag CB. Interstitial 125I radiosurgery of supratentorial de novo WHO Grade 2 astrocytoma and oligoastrocytoma in adults: long-term results and prognostic factors. Cancer. 2006;106(6):1372–81.
Bernstein M, Laperriere N, Glen J, Leung P, Thomason C, Landon AE. Brachytherapy for recurrent malignant astrocytoma. Int J Radiat Oncol Biol Phys. 1994;30(5):1213–7 [Clinical Trial].
Laperriere NJ, Leung PM, McKenzie S, Milosevic M, Wong S, Glen J, et al. Randomized study of brachytherapy in the initial management of patients with malignant astrocytoma. Int J Radiat Oncol Biol Phys. 1998;41(5):1005–11 [Clinical Trial Randomized Controlled Trial Research Support, Non-U.S. Gov’t].
Selker RG, Shapiro WR, Burger P, Blackwood MS, Arena VC, Gilder JC, et al. The Brain Tumor Cooperative Group NIH Trial 87-01: a randomized comparison of surgery, external radiotherapy, and carmustine versus surgery, interstitial radiotherapy boost, external radiation therapy, and carmustine. Neurosurgery. 2002;51(2):343–55. [Clinical Trial Comparative Study Randomized Controlled Trial Research Support, U.S. Gov't, P.H.S.]; discussion 55–7.
Ostertag CB. Brachytherapy–interstitial implant radiosurgery. Acta Neurochir Suppl (Wien). 1993;58:79–84 [Research Support, Non-U.S. Gov’t].
De Benedictis A, Moritz-Gasser S, Duffau H. Awake mapping optimizes the extent of resection for low-grade gliomas in eloquent areas. Neurosurgery. 2010;66(6):1074–84; discussion 84.
Suchorska B, Ruge M, Treuer H, Sturm V, Voges J. Stereotactic brachytherapy of low-grade cerebral glioma after tumor resection. Neuro Oncol. 2011;13(10):1133–42 [Clinical Trial].
Schupak K, Malkin M, Anderson L, Arbit E, Lindsley K, Leibel S. The relationship between the technical accuracy of stereotactic interstitial implantation for high grade gliomas and the pattern of tumor recurrence. Int J Radiat Oncol Biol Phys. 1995;32(4):1167–76.
Gabayan AJ, Green SB, Sanan A, Jenrette J, Schultz C, Papagikos M, et al. GliaSite brachytherapy for treatment of recurrent malignant gliomas: a retrospective multi-institutional analysis. Neurosurgery. 2006;58(4):701–9. [Comparative Study]; discussion 9.
Gobitti C, Borsatti E, Arcicasa M, Roncadin M, Franchin G, Minatel E, et al. Treatment of recurrent high-grade gliomas with GliaSite brachytherapy: a prospective mono-institutional Italian experience. Tumori. 2011;97(5):614–9 [Clinical Trial].
Welsh J, Sanan A, Gabayan AJ, Green SB, Lustig R, Burri S, et al. GliaSite brachytherapy boost as part of initial treatment of glioblastoma multiforme: a retrospective multi-institutional pilot study. Int J Radiat Oncol Biol Phys. 2007;68(1):159–65 [Evaluation Studies Multicenter Study].
Chino K, Silvain D, Grace A, Stubbs J, Stea B. Feasibility and safety of outpatient brachytherapy in 37 patients with brain tumors using the GliaSite Radiation Therapy System. Med Phys. 2008;35(7):3383–8.
Wu JS, Zhou LF, Tang WJ, Mao Y, Hu J, Song YY, et al. Clinical evaluation and follow-up outcome of diffusion tensor imaging-based functional neuronavigation: a prospective, controlled study in patients with gliomas involving pyramidal tracts. Neurosurgery. 2007;61(5):935–48. [Randomized Controlled Trial Research Support, Non-U.S. Gov't]; discussion 48-9.
Schumacher M. Long-term results of brachytherapy with temporary iodine-125 seeds in children with low-grade gliomas. Int J Radiat Oncol Biol Phys. 2011;80(5):1604. [Comment Letter]; author reply.
Schnell O, Scholler K, Ruge M, Siefert A, Tonn JC, Kreth FW. Surgical resection plus stereotactic 125I brachytherapy in adult patients with eloquently located supratentorial WHO grade II glioma - feasibility and outcome of a combined local treatment concept. J Neurol. 2008;255(10):1495–502.
Kreth FW, Faist M, Rossner R, Birg W, Volk B, Ostertag CB. The risk of interstitial radiotherapy of low-grade gliomas. Radiother Oncol. 1997;43(3):253–60 [Clinical Trial Controlled Clinical Trial].
Fabrini MG, Perrone F, De Franco L, Pasqualetti F, Grespi S, Vannozzi R, et al. Perioperative high-dose-rate brachytherapy in the treatment of recurrent malignant gliomas. Strahlenther Onkol. 2009;185(8):524–9.
Gutin PH, Prados MD, Phillips TL, Wara WM, Larson DA, Leibel SA, et al. External irradiation followed by an interstitial high activity iodine-125 implant “boost” in the initial treatment of malignant gliomas: NCOG study 6G-82-2. Int J Radiat Oncol Biol Phys. 1991;21(3):601–6 [Clinical Trial Multicenter Study Research Support, U.S. Gov’t, P.H.S.].
Wen PY, Alexander 3rd E, Black PM, Fine HA, Riese N, Levin JM, et al. Long term results of stereotactic brachytherapy used in the initial treatment of patients with glioblastomas. Cancer. 1994;73(12):3029–36 [Clinical Trial Research Support, U.S. Gov’t, P.H.S.].
Julow J, Kolumban Z, Viola A, Major T, Kolumban G. Prediction of volumetric change in the “triple ring” caused by glioma I-125 brachytherapy. Neuro Oncol. 2008;10(4):583–92 [Research Support, Non-U.S. Gov’t].
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Chaichana, K.L., Chen, L., Manrique-Guzman, S., Kleinberg, L., Quinones-Hinojosa, A. (2015). Management of Glial Tumors: Viewpoint—Surgery and Intra-cavitary Radiopharmaceutical Therapy. In: Chin, L., Regine, W. (eds) Principles and Practice of Stereotactic Radiosurgery. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-8363-2_18
Download citation
DOI: https://doi.org/10.1007/978-1-4614-8363-2_18
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-8362-5
Online ISBN: 978-1-4614-8363-2
eBook Packages: MedicineMedicine (R0)