Abstract
Acute coronary syndromes (ACS) frequently result from the rupture or erosion of a vulnerable coronary plaque, with associated intracoronary thrombosis. ACS also may occur in patients with angiographically normal coronary arteries. Some of these patients, however, still have angiographically silent underlying coronary artery disease. In this setting, subtle atherosclerotic changes frequently associated with unstable morphologic features or residual intracoronary thrombus may be detected with intracoronary imaging techniques. Nevertheless, other patients develop ACS as a result of nonatherosclerotic coronary artery disease (NA-CAD). ACS in patients with NA-CAD may be the consequence of coronary spasm or transient coronary embolic phenomena. In these patients, after the initial ischemic insult, late coronary angiography usually reveals normal epicardial coronary vessels. Kounis syndrome is a type of ACS generated by allergic reactions. Takotsubo cardiomyopathy is characterized by normal coronary arteries with a distinct pattern of transient left ventricular wall motion abnormalities. ACS also may occur in young patients following illicit drug use. Finally, spontaneous coronary artery dissection and intramural hematoma represent other etiologies of NA-CAD. In this review, we discuss current evidence regarding diagnostic and treatment strategies in patients presenting with ACS as a result of NA-CAD.




Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Maddox TM, Ho PM, Roe M, et al. Utilization of secondary prevention therapies in patients with nonobstructive coronary artery disease identified during cardiac catheterization. Circ Cardiovasc Qual Outcomes. 2010;3:632–41.
Berger JS, Elliot L, Gallup D, et al. Sex differences in mortality following acute coronary syndromes. JAMA. 2009;302:874–82.
Hochman JS, Tamis JE, Thompson TD, et al. Sex, clinical presentation and outcome in patients with acute coronary syndromes. N Engl J Med. 1999;341:226–32.
Gehrie ER, Reynolds HR, Chen AY, et al. Characterization and outcomes of women and men with non-ST-segment elevation myocardial infarction and nonobstructive coronary artery disease: results of the CRUSADE quality improvement initiative. Am Heart J. 2009;158:688–94.
Chokshi NP, Iqbal SN, Berger RL, et al. Sex and race are associated with the absence of epicardial coronary artery obstructive disease at angiography in patients with acute coronary syndromes. Clin Cardiol. 2010;33:495–501.
Amman P, Marschall S, Kraus M, et al. Characteristics and prognosis of myocardial infarction in patients with normal coronary arteries. Chest. 2000;117:333–8.
Mazurkiewicz L, Bilinska ZT, Kruk M, et al. Baseline clinical characteristics and midterm prognosis of STE-ACS and NSTE-ACS patients with normal coronary arteries. Ann Noninvasive Electrocardiol. 2009;14:4–12.
Reynols HR, Srichai MB, Iqbal SN, et al. Mechanisms of myocardial infarction in women without angiographically obstructive coronary artery disease. Circulation. 2011;124:1414–25. This prospective study evaluated IVUS and CMR findings in women with acute myocardial infarction and nonobstructive CAD.
Lanza GA, Sestito A, Sgueglia GA, et al. Current clinical features, diagnostic assessment and prognostic determinants of patients with variant angina. Int J Cardiol. 2007;118:41–7.
Takagi Y, Takahashi J, Yasuda S, et al. Prognostic stratification of patients with vasospastic angina. J Am Coll Cardiol. 2013;62:1144–53. The authors present a novel scoring system for the comprehensive risk assessment and prognostic stratification of patients with CV.
Manzano MC, Vilacosta I, San Roman JA, et al. Acute coronary syndrome in infective endocarditis. Rev Esp Cardiol. 2007;60:24–31.
Azzarelli S, Galassi AR, Amico F, et al. Clinical features of transient left ventricular apical ballooning. Am J Cardiol. 2006;98:1273–6.
Parodi G, Del Pace S, Carrabba N, et al. Incidence, clinical findings, and outcome of women with left ventricular apical ballooning syndrome. Am J Cardiol. 2007;99:182–5.
Sy F, Basraon J, Zheng H, et al. Frequency of Takotsubo cardiomyopathy in postmenopausal women presenting with an acute coronary syndrome. Am J Cardiol. 2013;112:479–82.
Sharkey SW, Windenburg DC, Lesser JR, et al. Natural history and expansive clinical profile of stress (tako-tsubo) cardiomyopathy. J Am Coll Cardiol. 2010;55:333–41.
Elesber AA, Prasad A, Lennon RJ, et al. Four-year recurrence rate and prognosis of the apical ballooning syndrome. J Am Coll Cardiol. 2007;50:448–52.
Feldman JA, Fish SS, Beshnsky JR, et al. Acute cardiac ischemia in patients with cocaine-associated complaints: results of a multicenter trial. Ann Emerg Med. 2000;36:469–76.
Hollander JE, Hoffman RS, Gennis P, et al. Cocaine Associated Chest Pain (COCHPA) Study Group. Prospective multicenter evaluation of cocaine-associated chest pain. Acad Emerg Med. 1994;1:330–9.
Alfonso F, Paulo M, Lennie V, et al. Spontaneous coronary artery dissection. Long term follow-up of a large series of patients prospectively managed with a “conservative” therapeutic strategy. J Am Coll Cardiol Intv. 2012;5:1062–70. In this large prospective series of patients with SCAD, a conservative therapeutic strategy provided an excellent long-term prognosis.
Vanzetto G, Berger-Coz E, Barone-Rochette G, Chavanon O, Bouvaist H, Hacini R, et al. Prevalence, therapeutic management and medium-term prognosis of spontaneous coronary artery dissection: results from a database of 11,605 patients. Eur J Cardiothorac Surg. 2009;35:250–4.
Tweet M, Hayes S, Pitta S, et al. Clinical features, management and prognosis of spontaneous coronary artery dissection. Circulation. 2012;126:579–88. This is the largest series with long follow-up in patients with SCAD.
Hill SF, Sheppard MN. Non-atherosclerotic coronary artery disease associated with sudden cardiac death. Heart. 2010;96:1119–25.
Dey S, Flather MD, Devlin G, et al. Sex-related differences in the presentation, treatment and outcomes among patients with acute coronary syndromes: the Global Registry of Acute Coronary Events. Heart. 2009;95:20–6.
Roe MT, Harrington RA, Prosper DM, et al. Clinical and therapeutic profile of patients presenting with acute coronary syndromes who do not have significant coronary artery disease. The Platelet Glycoprotein IIb/IIIa in Unstable Angina: Receptor Suppression Using Integrilin Therapy (PURSUIT) Trial Investigators. Circulation. 2000;102:1101–6.
Alfredsson J, Lindback J, Wallentin L, et al. Similar outcome with an invasive strategy in men and women with non-ST elevation acute coronary syndromes: from Swedish Web-System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies (SWEDEHEART). Eur Heart J. 2011;32:3128–36.
Prinzmetal M, Kennamer R, Merliss R, et al. Angina pectoris I: a variant form of angina pectoris; preliminary report. Am J Med. 1959;27:375–88.
Yasue H, Kugiyama K. Coronary spasm: clinical features and pathogenesis. Intern Med. 1997;36:760–5.
Yasue H, Nakagawa H, Itoh T, et al. Coronary artery spasm—clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008;51:2–17.
Kusama Y, Kodani E, Nakagomi A, et al. Variant angina and coronary artery spasm: the clinical spectrum, pathophysiology and management. J Nippon Med Sch. 2011;78:4–12.
Bastante-Valiente T, Gonzalez-Mansilla A, Parra-Fuertes JJ, et al. Sequential coronary spasm in Prinzmetal’s angina presenting as syncope. Rev Esp Cardiol. 2008;61:332–3.
Kishida H, Tada Y, Fukuma N, et al. Significant characteristics of variant angina patients with associated syncope. Jpn Heart J. 1996;37:317–26.
Romagnoli E, Lanza GA. Acute myocardial infarction with normal coronary arteries: role of coronary artery spasm and arrhythmic complications. Int J Cardiol. 2007;117:3–5.
Onaka H, Hirota Y, Shimada S, et al. Clinical observation of spontaneous angina attacks and multivessel spasm in variant angina pectoris with normal coronary arteries: evaluation by 24-hour 12-lead electrocardiography with computer analysis. J Am Coll Cardiol. 1996;27:38–44.
Okumura K, Yasue H, Horio Y, et al. Multivessel coronary spasm in patients with variant angina: a study with intracoronary injection of acetylcholine. Circulation. 1988;77:535–42.
Onaka H, Hirota Y, Shimada S, et al. Prognostic significance of the pattern of multivessel spasm in patients with variant angina. Jpn Circ J. 1999;63:509–13.
Akasaka T, Okumura K, Kawashima S, et al. Guidelines for the diagnosis and treatment of patients with vasospastic angina (coronary spastic angina) (JCS 2008). Circ J. 2008;72:1239–52.
Zaya M, Mehta PK, Merz BM. Provocative testing for coronary reactivity and spasm. J Am Coll Cardiol. 2014;63:103–8. This review of provocative testing for the diagnosis of CV summarizes various dosing protocols.
Hackett D, Larkin S, Chierchia S, et al. Induction of coronary artery spasm by a direct local action of ergonovine. Circulation. 1987;75:577–82.
Ong P, Athanasiadis A, Borgulya G, et al. Clinical usefulness, angiographic characteristics and safety evaluation of intracoronary acetylcholine provocation testing among 921 consecutive Caucasian patients with unobstructed coronary arteries. Circulation. 2014;129:1723–30.
Morikawa Y, Uemura S, Ishigami K, et al. Morphological features of coronary arteries in patients with coronary spastic angina: assessment with intracoronary optical coherence tomography. Int J Cardiol. 2011;146:334–40.
Tanaka A, Shimada K, Tearney GJ, et al. Conformational change in coronary artery structure assessed by optical coherence tomography in patients with vasospastic angina. J Am Coll Cardiol. 2011;58:1608–13.
Park HC, Choi SI, Lee JU, et al. Morphological findings in typical variant angina presenting as acute coronary syndrome using optical coherence tomography. J Interv Cardiol. 2013;26:491–500.
Morikawa Y, Mizuno Y, Harada E, et al. Aerobic interval exercise training in the afternoon reduces attacks of coronary spastic angina in conjunction with improvement in endothelial function, oxidative stress, and inflammation. Coron Artery Dis. 2013;24:177–82.
Nishigaki K, Inoue Y, Yamanouchi Y, et al. Prognostic effects of calcium channel blockers in patients with vasospastic angina—a meta analysis. Circ J. 2010;74:1943–50.
Kounis NG, Zavras GM. Histamine-induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract. 1991;45:121–8.
Kounis NG. Coronary hypersensitivity disorder: the Kounis syndrome. Clin Ther. 2013;35:563–71. This recent review of KS was written by the author who first described the association between ACS and allergic reactions.
Kounis NG, Mazarakis A, Tsigkas G, et al. Kounis syndrome: a new twist on an old disease. Futur Cardiol. 2011;7:805–24.
Chen JP, Hou D, Pendyala L, et al. Drug-eluting stent thrombosis: the Kounis hypersensitivity-associated acute coronary syndrome revisited. JACC Cardiovasc Interv. 2009;2:583–93.
Rico-Cepeda P, Palencia-Herrejon E, Rodriguez Aguirregabiria MM. Kounis syndrome. Med Intensiv. 2012;36:358–64.
Cevik C, Nugent K, Shome GP, et al. Treatment of Kounis syndrome. Int J Cardiol. 2010;143:223–6.
Tang L, Hu XQ, Zhou SH. Coronary artery embolism causing acute myocardial infarction in patients with mechanical heart valve prosthesis: which is the optimal treatment? Heart Lung Circ. 2013;23(5):422–7.
López-Lluva MT, Sánchez-Pérez I, Fernández-Vallejo V, et al. Non-atherosclerotic acute myocardial infarction: coronary artery embolism. Med Intensiv. 2013;31:209–11.
Czarina JR, Weekes AJ. Acute myocardial infarction caused by coronary embolism from infective endocarditis. J Emerg Med. 2011;40:509–14.
Bathina JD, Daher IN, Plana JC, et al. Acute myocardial infarction associated with nonbacterial thrombotic endocarditis. Tex Heart Inst J. 2010;37:208–12.
Angulo-Llanos R, Sanz-Ruiz R, Solis J, et al. Acute myocardial infarction: an uncommon complication of takotsubo cardiomyopathy. Catheter Cardiovasc Interv. 2013;82:909–13.
Han DC, Kim JS, Lee SK, et al. Native aortic valve thrombosis: an unusual cause of acute ST-elevation myocardial infarction. Cardiovasc Pathol. 2013;22:e23–6.
Hisatomi K, Yamada T, Odate T, et al. Intermittent coronary artery occlusion caused by a floating thrombus in the left coronary sinus of Valsalva of a patient with a normal aorta and protein C deficiency. Ann Thorac Surg. 2011;92:1508–10.
Ferreira AR, Freitas A, Magno P, et al. Acute coronary syndrome of paradoxical origin. Rev Port Cardiol. 2013;32:817–21.
Myers PO, Bounameaux H, Panos A, et al. Impending paradoxical embolism. Chest. 2010;137:164–70.
Brito JD, Almeida MS, Ribeiras R, et al. Recurrent myocardial infarction in a patient with papillary fibroelastoma. Arq Bras Cardiol. 2012;98:e7–10.
Konstanty-Kalndyk J, Wierzbicki K, Bartus K, et al. Acute myocardial infarction due to coronary embolisation as the first manifestation of left atrial myxoma. Kardiol Pol. 2013;71:403–5.
Protasiewick M, Rojek A, Gajek J, et al. Cardiac arrest due to left circumflex coronary artery embolism as a complication of subtherapeutic oral anticoagulation in a patient with mitral and aortic mechanical valve prostheses. Postep Kardiol Int. 2013;9:97–100.
Sato HTH, Tateishi H, Uchido T, et al. Takotsubo type cardiomyopathy due to multivessel spasm. In: Kodama K, Haze K, Hon M, editors. Clinical aspect of myocardial injury: from ischemia to heart failure (in Japanese). Tokyo: Kagakuhyouronsya Co.; 1990. p. 56–64.
Desmet WJ, Adriaenssens BF, Dens JA. Apical ballooning of the left ventricle: first series in white patients. Heart. 2003;89:1027–31.
Schneider B, Athanasiadis A, Stölberger C, et al. Gender differences in the manifestation of tako-tsubo cardiomyopathy. Int J Cardiol. 2013;166:584–8.
Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155:408–17.
Ghadri JR, Ruschitzka F, Lüscher TF, Templin C. Takotsubo cardiomyopathy: still much more to learn. Heart. 2014. doi:10.1136/heartjnl-2013-304691. The authors present an up-to-date review on TTC.
Nguyen TH, Neil CJ, Sverdlov AL, et al. N-terminal pro-brain natriuretic protein levels in takotsubo cardiomyopathy. Am J Cardiol. 2011;108:1316–21.
Lozano A, Bastante T, Salamanca J, et al. Tako-Tsubo cardiomyopathy triggered by influenza A virus infection. Int J Cardiol. 2014. doi:10.1016/j.ijcard.2014.04.033.
Alfonso F, Núñez-Gil IJ, Hernández R. Optical coherence tomography findings in Tako-Tsubo cardiomyopathy. Circulation. 2012;126:1663–4.
Alfonso F, Cárdenas A, Ibáñez B, et al. Mid-ventricular tako-tsubo cardiomyopathy with structurally normal coronary arteries confirmed by optical coherence tomography. J Invasive Cardiol. 2013;25:e214–5.
Eitel I, von Knobelsdorff-Brenkenhoff F, Bernhardt P, et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. JAMA. 2011;306:277–86. In this prospective multicenter registry of patients with TTC, CMR was used systematically at initial presentation and follow-up.
Santoro F, Ieva R, Ferraretti A, et al. Safety and feasibility of levosimendan administration in takotsubo cardiomyopathy: a case series. Cardiovas Ther. 2013;31:e133–7.
Santoro F, Ieva R, Musaico F, et al. Lack of efficacy of drug therapy in preventing takotsubo cardiomyopathy recurrence: a meta-analysis. Clin Cardiol. 2014;37(7):434–9.
US Department of Health and Human Services (DHS); Office of Applied Studies. Results from the 2008 National Survey on Drugs Use and Health: national findings. http://oas.samshsa.gov/nsduh/2k8nsduh/2k8Results.cfm.
US Department of Health and Human Services (DHS), Substance Abuse and Mental Health Service Administration, Office of Applied Studies. Drug Abuse Warning Network, 2007: national estimates of drug-related emergency department visits. Rockville, MD: 2010. https://dawninfo.smhsa.gov/files/ED2007/DAWN2k7ED.pdf
Burillo-Putze G, Borreguero León JM, García Dopico JA, et al. Incidence and impact of undisclosed cocaine use in emergency department chest pain and trauma patients. Int J Emerg Med. 2008;1:169–72.
Brogan III WC, Lange RA, Kim AS, et al. Alleviation of cocaine-induced coronary vasoconstriction by nitroglycerin. J Am Coll Cardiol. 1991;18:581–6.
Moliterno DJ, Willard JE, Lange RA, et al. Coronary-artery vasoconstriction induced by cocaine, cigarette smoking, or both. N Engl J Med. 1994;330:454–9.
Dressler FA, Malekzadeh S, Roberts WC. Quantitative analysis of amounts of coronary arterial narrowing in cocaine addicts. Am J Cardiol. 1990;65:303–8.
Finkel JB, Marhefka GD. Rethinking cocaine-associated chest pain and acute coronary syndromes. Mayo Clin Proc. 2011;86:1198–207. This review focuses on the relationship between cocaine abuse and ACS.
Hollander JE, Levitt MA, Young GP, et al. Effect of recent cocaine use on the specificity of cardiac markers for diagnosis of acute myocardial infarction. Am Heart J. 1998;135:245–52.
McCord J, Jneid H, Hollander JE, et al. Management of cocaine-associated chest pain and myocardial infarction: a scientific statement from the American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology. Circulation. 2008;117:1897–907.
Dattilo PB, Hailperm SM, Fearon K, et al. Beta-blockers are associated with reduced risk of myocardial infarction after cocaine use. Ann Emerg Med. 2008;51:117–25.
Rangel C, Shu RG, Lazar LD, et al. Beta-blockers for chest pain associated with recent cocaine use. Arch Intern Med. 2010;170:874–9.
Hoskins MH, Leleiko RM, Ramos JJ, et al. Effects of labetalol on hemodynamic parameters and soluble biomarkers of inflammation in acute coronary syndrome in patients with active cocaine use. J Cardiovasc Pharmacol Ther. 2010;15:47–52.
Pretty H. Dissecting aneurysms of coronary artery in woman aged 42: rupture. BMJ. 1931;1:667.
Alfonso F. Spontaneous coronary artery dissection. New insights from the tip of the iceberg? Circulation. 2012;126:667–70.
Saw J, Ricci D, Starovoytov A, et al. Spontaneous coronary artery dissection. Prevalence and predisposing conditions including fibromuscular dysplasia in a tertiary center cohort. J Am Coll Cardiol Intv. 2013;6:44–52. Patients with SCAD were prospectively and retrospectively screened for fibromuscular dysplasia. The results show a high prevalence of concomitant fibromuscular dysplasia in these patients.
Vrints C. Spontaneous coronary artery dissection. Heart. 2010;96:801–8.
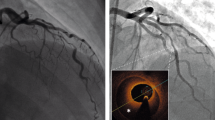
Alfonso F, Paulo M, Gonzalo N, et al. Diagnosis of spontaneous coronary artery dissection by optical coherence tomography. J Am Coll Cardiol. 2012;59:1073–9.
Compliance with Ethics Guidelines
Conflict of Interest
Amparo Benedicto, Teresa Bastante, Jorge Restrepo, Javier Cuesta, Fernando Rivero, and Fernando Alfonso have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Management of Acute Coronary Syndromes
Rights and permissions
About this article
Cite this article
Bastante, T., Rivero, F., Cuesta, J. et al. Nonatherosclerotic Causes of Acute Coronary Syndrome: Recognition and Management. Curr Cardiol Rep 16, 543 (2014). https://doi.org/10.1007/s11886-014-0543-y
Published:
DOI: https://doi.org/10.1007/s11886-014-0543-y