Abstract
Rationale:
Although health surveys are routinely used to estimate the population incidence and prevalence of many chronic and acute conditions in the U.S. population, they have infrequently been used for “rare” conditions such as primary immunodeficiency diseases (PID). Accurate prevalence measures are needed to separate the truly rare condition from those that primary care doctors are likely to see in their practices today, if early diagnosis and treatment are to be achieved.
Methods:
A national probability sample of 10,000 households was sampled by random digit dialing and screened by telephone to identify how many of the nearly 27,000 household members had been diagnosed with a PID.
Results:
A total of 23 household members in 18 households were reported with a specific diagnosis for PID (CVID, IgA, IgG, XLA, SCID, CGD), whereas additional cases were reported as a PID without a confirmatory diagnosis. These findings suggest a population prevalence of diagnosed PID in the United States at approximately 1 in 1,200 persons.
Conclusions:
Diagnoses of PID in the United States are far more common than suggested in the literature.
Similar content being viewed by others
Introduction
Primary immunodeficiency diseases (PID) represent a class of disorders in which there is an intrinsic defect in the human immune system (rather than immune disorders that are secondary to infection, chemotherapy or some other external agent). In some cases, the body fails to produce any or enough antibodies to fight infection. In other cases, the cellular defenses against infection fail to work properly. There are more than 150 different PID currently recognized by the World Health Organization [1].
Although PID are often described as rare disorders, the true incidence or population prevalence of these diseases, either individually or in the aggregate, are not known because there is no screening for these defects at birth or at any time during life anywhere in the world. The major health surveys conducted by the government in the United States, the National Health Interview Survey, and the National Health and Nutrition Examination Survey do not collect information on PID. No comprehensive population survey has even been undertaken by the federal government to estimate the incidence, prevalence or population characteristics of these diseases in the United States. Hence, although these diseases are clinically described in the medical literature, and there have been some estimates of the incidence and prevalence of some disorders based on primary immunodeficiency registries in various countries, [2–28] there are no data based on population screening of either the incidence or prevalence of these conditions in the United States.
The objectives of the survey reported here were to (1) estimate the population prevalence of PID in the United States based on community samples rather than clinical samples, using a national probability sampling frame so that population size can be estimated, and (2) compare the characteristics of a true national sample of PID patients to previous surveys of patients within the Immune Deficiency Foundation.
Methods
A telephone survey was conducted with adult informants in a national random digit dialing (RDD) sample of 10,005 households. The sample size was selected to detect the lowest expected prevalence rate for diagnosed PID in the United States. This was based on the results of the First Immune Deficiency Foundation (IDF) National Patient Survey of medical specialists in 1995, which identified 1,502 doctors who reported following-up a total of 21,312 patients with PID diagnoses. Because only 2,616 (15.0%) out of 17,451 specialists responded to the survey and only selected specialists were covered by the sampling frame, these 21,312 cases should represent only a fraction of the total number of diagnosed cases in the United States. However, if they represented all diagnosed cases of PID in the United States in 1995, then the population prevalence would be 0.8 cases per 10,000 persons. Hence, a national sample of 10,000 households with an average of 2.7 persons per household would be large enough to detect the lowest expected prevalence for diagnosed PID in the U.S. population.
The sample was geographically stratified by time zone. The survey was conducted by experienced interviewers using computer-assisted telephone interviewing (CATI) from a central facility. Initial contact attempts were made on evenings and weekends. Up to four follow-up contact attempts were made to complete an interview. Interviews were conducted between July 26 and August 25, 2005. A cooperation rate (completes/completes+refusals) of 80% was achieved.
An adult informant enumerated the adults and children in the household. A total of 19,884 adults and 6,773 children or 26,657 persons were reported in these households. This provides a denominator for estimates of the prevalence of PID among adults and children in these households. If there were children in the household, respondents were asked if any of the children had a chronic or serious health condition and, if so, what the condition was. All respondents were asked: “Has anyone in your household ever been diagnosed with a primary immunodeficiency disease, such as common variable immunodeficiency, IgA deficiency, IgG subclass deficiency or any other immunodeficiency? (This is not acquired immunodeficiency—AIDS).” The question included the three most common diagnoses of PID patients in the Second IDF National Survey of Patients in 2002, which represented approximately three quarters of those in that survey. If the respondents in the household surveyed answered “yes”, they were asked the number of persons in the household with a primary immunodeficiency, their age, gender, and specific type of primary immunodeficiency. A limited set of additional questions were asked about treament and contact.
Results
A total of 342 (10%) out of 3,478 households with children aged 17 years old or younger reported that 1 or more children in the household had a serious or chronic health condition. Out of 6,773 children in these households, 4 were reported to have an immunodeficiency disease. However, in response to a follow-up question about the specific diagnosis, one of these cases had been diagnosed with ITP, an autoimmune disorder. The other three children were reported to have diagnoses that are PID: agammaglobulinemia, selective IgA deficiency, and IgG subclass deficiency.
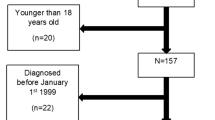
All household informants were then asked: “Has anyone in your household ever been diagnosed with a primary immunodeficiency disease, such as common variable immunodeficiency, IgA deficiency, IgG subclass deficiency or any other immunodeficiency? (This is not acquired immunodeficiency—AIDS).” In 131 (1.3%) out of 10,005 households surveyed, the household informant reported that someone in the household had been diagnosed with a PID (Fig. 1). However, when asked the specific diagnosis for the condition, most (66%) reported a diagnosis other than a primary immunodeficiency (Table 1). In many of these cases, the diagnosed condition was either an autoimmune disease or one that had an immunological component. Half of the remaining cases either had no diagnosis given (16%) or the condition could not be classified from the description (3%) (Fig. 2).
Nonetheless, a total of 23 household members in 18 households were reported with a specific diagnosis for PID (CVID, IgA, IgG, XLA, SCID, CGD) (Fig. 3). These findings suggest a population prevalence of diagnosed PID at 1 in 1,200 persons in the United States. This translates into a population rate for diagnosed PID of 0.0863%. When applied to the U.S. population of 297,386,000 persons, this gives an estimate of approximately 250,000 persons with diagnosed PID in the United States. The confidence bounds about this estimate at the 95% confidence level suggest that the number of persons with the diagnoses of PID in the United States will be between 152,000 and 361,000 (Table 2).
The population characteristics of this national probability sample of persons diagnosed with PID can be compared to two earlier large scale, nationally distributed but nonprobability surveys of patients conducted by the Immune Deficiency Foundation in 1996–1997 (N = 3,046) and 2002 (N = 1,526). The first IDF survey of patients was distributed through physicians and medical centers known to the Foundation to be treating patients (First Patient Survey) [29]. The second IDF survey of patients was mailed to patients on IDF’s mailing list who had not participated in the first survey (Second Patient Survey) [30].
The proportion of males in the national probability sample (56%) is somewhat higher than in the first IDF survey (48%) and the second IDF survey (42%). The proportion of patients under 18 years of age in the national probability sample (43%) falls between the proportion under 18 years of age in the first IDF survey (40%) and the second IDF survey (50%) (Fig. 4). In general, the age and gender distribution of the probability sample is consistent with the characteristics of patients known to the foundation.
The current Clinical Care Guidelines for Patients with Primary Immunodeficiency Diseases recommend treatment with intravenous immunoglobulin (IVIG) for agammaglobulinemia, common variable immunodeficiency, hyper IgM, Wiskott–Aldrich, and severe combined immunodeficiency. Specific antibody deficiency, which may be a part of IgG subclass deficiency, is also indicated although IgG subclass deficiency alone is not. The majority of the patients in the probability sample (57%) have diagnoses for which IVIG therapy is the standard of care. This is similar to the proportion of patients in the second IDF survey with diagnoses for which IVIG is the standard of care (65%). However, only 22% of PID patients in the national household telephone survey sample were currently being treated with IVIG compared to 67% of PID patients in the second IDF survey. Indeed, only 67% of patients with aggammaglobulinemia and 13% of patients with common variable immunodeficiency in the national probability sample were currently being treated with IVIG (Fig. 5). Hence, the surveys suggest that immune deficient patients known to the IDF, either through referral by specialist or individual information-seeking are more likely to be following the recommended therapy for the condition than the average patient in the general community.
The national telephone survey confirmed that, despite an IDF mailing list of more than 10,000 diagnosed PID patients, only 4 out of 18 households containing a total of 23 PID patients in a national probability sample had ever heard of the Foundation, and only 1 out of 18 received the IDF newsletter. If the rate of 1 out of 18 households with a patient receiving a newsletter is divided into the IDF newsletter mailing list of 10,000, it yields an independent estimate of 180,000 households with patients diagnosed with a PID. If this household estimate is converted to a population estimate of 1.3 patients per household (23/18), then the survey yields an independent national estimate of approximately 230,000 persons diagnosed with a PID.
Discussion
PID are far more common than previously estimated. The survey suggests prevalence rates for diagnosed PID as 1 in 2,000 for children, 1 in 1,200 for all persons, and 1 in 600 households. The population prevalence for PID found among children in this survey replicates earlier unpublished findings from large scale community surveys. The population prevalence found in the survey presented here would yield a total population estimate of between 150,000 and 360,000 persons in the United States diagnosed with PID.
Population characteristics of PID patients in the national survey (age, gender) are similar to those in previous patient surveys conducted by IDF. The distribution of PID patients by diagnosis for which IVIG is the current standard of care is similar for the national probability survey (57%) and the most recent patient survey (65%). However, current use of IVIG by PID patients in the national probability survey (22%) was far lower than in previous IDF patient surveys (67%), and the difference is statistically significant. If PID patients in the general population used IVIG at the rates used by patients in previous IDF surveys, there would be a major increase in demand.
Neither the true incidence nor true prevalence of PID is known. Whereas there have been estimates of these parameters from geographically limited studies [4, 8, 11, 13, 21, 26]; those estimates were based on diagnosed cases. The number of undiagnosed cases is not known because there is no population-based screening process for PID anywhere in the world at any time during life. Underdiagnosis also occurs because autopsies are rarely performed on infants or children who die from infections. Moreover, as some individuals may have less severe forms of primary immunodeficiency that allow them to survive, they are often not diagnosed early in life or at all.
Conclusions
In conclusion, these data suggest that PID are not rare. The true incidence and prevalence of these conditions will never be known until there is newborn or population screening for these defects. Usually, the only way one knows that an underlying immunodeficiency exists is that the patient develops recurrent or serious infections and is then tested for these defects. These patients appear outwardly normal in most cases so that their appearances usually do not trigger a suspicion of immunodeficiency. Occasionally, the diagnosis is made before infections set in when there is a family history of such defects and family members are screened. Blood banks also often test both donors and recipients for IgA deficiency because that condition is often accompanied by the production of antibodies to IgA, which can cause transfusions reactions. In one such blood bank survey, the incidence was 1:333 putatively normal blood donors [7]. The current study suggests that these conditions are sufficiently common that primary care physicians are likely to see patients with underlying primary immunodeficiency disorders in their practice and should test for these disorders in patients with recurring, unusual or serious infections. In the absence of routine screening, physician awareness of the relative frequency of these disorders is critical to early diagnosis and treatment.
References
Notarangelo L, Casanova JL, Conley ME, Chapel ME, Fischer A, Puck J et al. Primary immunodeficiency diseases: an update from the International Union of Immunological Societies Primary Immunodeficiency Diseases Classification Committee Meeting in Budapest, 2005. J Allergy Clin Immunol 2006;117:883–96.
Ryser O, Morell A, Hitzig WH. Primary immunodeficiencies in Switzerland: first report of the national registry in adults and children. J Clin Immunol 1988;8:479–85.
Mila J, Matamoros N, Pons de Ves J, Raga S, Iglesias Alzueta J. [The Spanish Registry of primary immunodeficiencies. REDIP-1998]. Sangre (Barc) 1999;44:163–7.
Golan H, Dalal I, Garty BZ, Schlesinger M, Levy J, Handzel Z et al. The incidence of primary immunodeficiency syndromes in Israel. Isr Med Assoc J 2002;4:868–71.
Aghamohammadi A, Moein M, Farhoudi A, Pourpak Z, Rezaei N, Abolmaali K et al. Primary immunodeficiency in Iran: first report of the national registry of PID in children and adults. J Clin Immunol 2002;22:375–80.
Affentranger P, Morell A, Spath P, Seger R. Registry of primary immunodeficiencies in Switzerland. Immunodeficiency 1993;4:193–5.
Clark JA, Callicoat PA, Brenner NA. Selective IgA deficiency in blood donors. Am J Clin Pathol 1983;80:210–3.
Fasth A. Immunodeficiency in children in Sweden (1974–1983). J Clin Immunol 1982;2:86–92.
Sullivan KE, Mullen CA, Blaese RM, Winkelstein JA. A multi-institutional survey of the Wiskott–Aldrich syndrome. J Pediatr 1994;125:876–85.
Winkelstein JA, Marino MC, Johnston RB Jr, Boyle J, Curnutte J, Gaillin JI et al. Chronic granulomatous disease. Report on a national registry of 368 patients. Medicine (Baltimore) 2000;79:155–69.
Lim DL, Thong BY, Ho SY, Shek LP, Lou J, Leong K et al. Primary immunodeficiency diseases in Singapore—the last 11 years. Singap Med J 2003;44:579–86.
Montoya CJ, Henao J, Salgado H, Olivares MM, Lopez JA, Rugeles C et al. [Phenotypic diagnosis of primary immunodeficiencies in Antioquia, Colombia, 1994–2002]. Biomedica 2002;22:510–8.
Stray-Pedersen A, Abrahamsen TG, Froland SS. Primary immunodeficiency diseases in Norway. J Clin Immunol 2000;20:477–85.
Javier FC III, Moore CM, Sorensen RU. Distribution of primary immunodeficiency diseases diagnosed in a pediatric tertiary hospital. Ann Allergy Asthma Immun 2000;84:25–30.
Zelazko M, Carneiro-Sampaio M, Cornejo de Luigi M, Garcia de Olarte D, Porras Madrigal O, Berron Perez R et al. Primary immunodeficiency diseases in Latin America: first report from eight countries participating in the LAGID. Latin American Group for Primary Immunodeficiency Diseases. J Clin Immunol 1998;18:161–6.
Eley BS, Hughes J, Cooper M, Pienaar S, Beatty DW. Primary immunodeficiency diseases at Red Cross War Memorial Children’s Hospital. S Afr Med J 1997;87:1684–8.
Bejaoui M, Barbouche MR, Sassi A, Larguche B, Miladi N, Bouguerra A et al. [Primary immunodeficiency in Tunisia: study of 152 cases]. Arch Pediatr 1997;4:827–31.
Baumgart KW, Britton WJ, Kemp A, French M, Roberton D. The spectrum of primary immunodeficiency disorders in Australia. J Allergy Clin Immunol 1997;100:415–23.
Grumach AS, Duarte AJ, Bellinati-Pires R, Pastorino AC, Jacob CM, Diogo CL et al. Brazilian report on primary immunodeficiencies in children: 166 cases studied over a follow-up time of 15 years. J Clin Immunol 1997;17:340–5.
Matamoros FN, Mila LJ, Espanol BT, Raga BS, Fontan CG. Primary immunodeficiency syndrome in Spain: first report of the national registry in children and adults. J Clin Immunol 1997;17:333–9.
Nunez RM. Primary immunodeficiency in Colombian children. Allergol Immunopathol (Madr) 1988;16:273–5.
Bernatowska E, Madalinski K, Michalkiewicz J, Gregorek H. Primary immunodeficiency diseases in children treated in the Children’s Memorial Hospital, Poland. Immunol Invest 1988;17:107–20.
Datta U, Kumar L, Mehta S, Walia BN, Sharma BK, Sehgal S et al. Primary immunodeficiency defects seen in PGI—one year study. J Assoc Phys India 1984;32:701–04.
Luzi G, Businco L, Aiuti F. Primary immunodeficiency syndromes in Italy: a report of the national register in children and adults. J Clin Immunol 1983;3:316–20.
Luzi G, Businco L, Aiuti F. A national registry for primary immunodeficiency syndromes in Italy: a report for the period 1972–1982. Birth Defects Orig Artic Ser 1983;19:161–3.
Hayakawa H, Iwata T, Yata J, Kobayashi N. Primary immunodeficiency syndrome in Japan. I. Overview of a nationwide survey on primary immunodeficiency syndrome. J Clin Immunol 1981;1:31–9.
Leiva LE, Zelazco M, Oleastro M, Carneiro-Sampaio M, Condino-Neto A, Costa-Carvalho BT et al. Primary immunodeficiency diseases in Latin America: the second report of the LAGID registry. J Clin Immunol 2007;27:101–8.
Rezaei N, Aghamohammadi A, Moin M, Pourpak Z, Movahedi M, Gharagozlu M et al. Frequency and clinical manifestations of patients with primary immunodeficiency disorders in Iran: update from the Iranian Primary Immunodeficiency Registry. J Clin Immunol 2006;26:519–32.
Immune Deficiency Foundation. Primary immune deficiency diseases in America: the first national survey of patients and specialists. 1999 http://www.primaryimmune.org/pubs/IDF_survey_complete.pdf
Immune Deficiency Foundation. Primary immune deficiency diseases in America: the second national survey of patients and specialists. 2003 http://www.primaryimmune.org/pubs/IDF_survey_complete.pdf
Acknowledgement
The survey was conducted for the Immune Deficiency Foundation, a nonprofit patient organization, through the generous support of a grant from Talecris Biotherapeutics.
Author information
Authors and Affiliations
Corresponding author
Additional information
Schulman, Ronca & Bucuvalas Inc. (SRBI) for the Immune Deficiency Foundation.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Boyle, J.M., Buckley, R.H. Population Prevalence of Diagnosed Primary Immunodeficiency Diseases in the United States. J Clin Immunol 27, 497–502 (2007). https://doi.org/10.1007/s10875-007-9103-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-007-9103-1