Abstract
Repeated invasive procedures occur routinely in neonates who require intensive care, causing pain at a time when it is developmentally unexpected. Multiple lines of evidence suggest that repeated and prolonged pain exposure alters their subsequent pain processing, long-term development, and behaviour. Primary outcome of this study was to evaluate the reduction of procedural pain induced by “heel-lances” in preterm newborns with three different treatment [administration of fentanyl (FE, 1–2 μg/kg), facilitated tucking (FT), sensorial saturation (SS)]. Secondary outcome was the measurement of the levels of cytokines as markers of stress correlated to pain. A prospective randomized controlled trial (RCT) comparing three different pharmacological or non-pharmacological treatments was performed involving 150 preterm newborn (gestational age 27–32 weeks). No other analgesic treatment was performed during the study. CRIES score was used to evaluate the procedural pain. The results showed that the reduction in the pain score was greater in FE and SS groups than FS group. The differences were statistically significant (p < 0.01). The levels of IL-6, IL-8, and TNF-α were higher in the FT individuals than in the FE or SS-treated infants at 1 day (p < 0.01), at 3 days (p < 0.01), and at 7 days (p < 0.01) of life. Conclusions: The findings of this study suggest that FE and SS provide a superior analgesia in preterm neonates during procedural pain. In particular, sensorial saturation seems to be an important non-pharmacological alternative treatment to prevent and reduce the procedural pain in preterm newborn.
Similar content being viewed by others
Introduction
Repeated invasive procedures occur routinely in neonates who require intensive care, causing pain at a time when it is developmentally unexpected [8]. Neonates are more sensitive to pain than older infants, children, and adults [4], and this hypersensitivity is further exacerbated in preterm neonates [13, 27].
Multiple lines of evidence suggest that repeated and prolonged pain exposure in infants alters subsequent pain processing, long-term development, and behaviour [28, 32]. Neonatal pain has psychological [6, 62] and physical consequences, provoking hypoxemia, hypertension, tachycardia, a rise of heart rate variability, and of intracranial pressure [42, 52]. In the preterm, infant pain may cause brain damage [4], in concurrence with the immature vasoregulation of the premature central nervous system [56]. It has been demonstrated that anesthetizing newborns before surgery reduces neurological damage [2, 4].
Research in adults has demonstrated that plasma levels of variety of hormones including corticosteroids, cathecholamines, growth hormone, and insulin change in response to emotionally and physically stressful stimuli [1, 30, 38].
Cytokines are soluble proteins secreted mainly by immune cells and are key players in the induction and maintenance of pain. Proinflammatory cytokines are mostly algesic, while antiinflammatory cytokines have analgesic properties. After the role of cytokines was shown in diverse animal models of pain, interest rose in terms of the systemic and local regulation of cytokines in human pain states [57].
Numerous pharmacological and non-pharmacological treatments can alleviate procedural pain in neonates. As an example, opiates are potent analgesics which have been shown to have an effect on stress responses; when these agents are used in surgery they improve important medical outcomes [3]. Opiates have been shown to reduce physiological instability in the newborn in several ways. Studies have variously demonstrated that with opiates there is less hypoxaemia [31, 44], less blood pressure fluctuation [57], reduced behavioural and hormonal stress response [9, 43], and elevated ventilator synchrony [26]. Conflicting evidence exists about the efficacy of continuous morphine infusions to relieve pain from routine procedures among preterm neonates in neonatal (Neonatal Intensive Care Units, NICU). Anand et al. [5] found a reduction in pain scores, whereas some other studies have found no effect of morphine infusions on poor neurological outcomes and minor effects on pain scores [7, 49]. Continuous infusion of morphine, studied in large RCTs, was not recommended for routine use in premature infants [16]. Fentanyl and morphine are equally effective in terms of analgesia, but the first one has fewer side effects than other one, in particular as regards the reduced gastrointestinal motility and hemodynamic stability [48].
A number of non-pharmacologic therapies are beneficial to the management of mild to moderate pain in the neonate [37]. These therapies include non-nutritive sucking both with and without sucrose, swaddling or kangaroo care, music therapy, and multi-sensorial saturation. Positioning infants to provide containment that maintains a flexed position either with blanket rolls or via “facilitated tucking” (holding the infant with extremities flexed and close to trunk) helps facilitate self-regulation and decreased crying time during heel sticks [21, 54].
Sensorial saturation (SS), i.e., the use of various non-painful stimuli, is based on competition of various gentle stimuli, given during the painful event, with the transmission of pain to the central nervous system [11–14]. These stimuli (tactile, auditory, olfactory, and visual) increase the analgesic effect of oral sugar. They have analgesic actions in both preterm [11] and term babies [12].
The primary outcome of the current study was to evaluate the reduction of procedural pain induced by heel-lance procedures in preterm newborns with three different pharmacological or non-pharmacological treatments [administration of fentanyl (FE), facilitated tucking (FT), SS]. Secondary outcome was the measurement of the levels of cytokines during the same painful procedure, which served as markers of stress correlated to pain.
Methods
Population
This study was a prospective, randomized, controlled trial, which was conducted between September 2007 and September 2009 in a group of 150 newborns with gestational age from 27 to 32 weeks admitted to the Neonatal Intensive Care Unit at the Policlinic of the University of Messina. The study was approved by the Ethical Committee and performed only if parental consent was obtained. All performed procedures during the study were clinically useful. Exclusion criteria were the presence of an infectious disease, congenital malformations of the brain, or inborn errors of metabolism.
The primary outcome of the study was to evaluate the utility of three different pharmacological or non-pharmacological treatments to alleviate the procedural pain due to heel-lances performed within 2 days of birth. The secondary outcome was the level of cytokines [interleukin6 (IL-6), interleukin 8 (IL-8), and tumour necrosis factor (TNF-α)] during the painful procedures. All procedures were performed by certified nurses or physicians, as per standard practices at the study centre.
Babies were enrolled consecutively in the study and were divided randomly into 3 groups, each of 50 newborns, according to the type of analgesia used: administration of opioids (FE at a dose of 1–2 μg/kg), FT, and SS. Roughly 5 min before each procedure, a portable pulse oximeter was applied to the newborn’s foot or hand. All neonates had umbilical venous and arteriosus catheters for 7 days and were in a supine position and partially swaddled (the limb that was used for the procedure was exposed). Parents were present during the procedure but did not touch or interact with their newborn. For the newborns that received fentanyl, 2 min prior to every painful heel lance procedure within 2 days of life a bolus injection of the drug was administered intravenously. For the FT group, before every heel-lance procedure within 2 days of life, the infant was positioned with extremities flexed and close to trunk. For the newborns enrolled in the SS group, before every procedure, treatment consisted of simultaneously: (1) lying the infant on its side, with legs and arms flexed but free to move; (2) looking the infant in the face, close up, to attract his attention; (3) massaging the infant’s face and back; (4) speaking to the infant gently, but firmly; (5) letting the infant smell the fragrance of the baby oil (Babygella, Guieu Labs) on the therapist’s hands; and (6) instilling 10% glucose on the infant’s tongue with the same timing and method described for FT intervention.
No other analgesic treatment was performed during the 7 days of study. Between Days 2 and 7, infants were treated with standard neonatal intensive care.
Pain assessment
Pain was assessed using a validated composite pain measure, the CRIES Score (C—Crying; R—Requires increased oxygen administration; I—Increased vital signs; E—Expression; S—Sleeplessness). The CRIES, a neonatal method for measurement of postoperative pain, was based on a thorough review of the literature, used a 10-point scale similar to the APGAR (appearance, pulse, grimace, activity and respiration) score, and was developed as an acronym to facilitate remembrance for clinical use [40, 53]. The minimal and maximal scores for the CRIES are 0 and 10, respectively. A score equal to or less than 5 indicates no pain; a score greater than 5 indicates the procedure was painful. The CRIES tool was chosen because it includes both behavioural and physiological scores [40]. The CRIES responses were assessed by trained nurses and physicians during every heel-lance procedures.
Blood samples
Blood samples were collected from each newborn included in the study before any procedure and at 1, 3, and 7 days of life. Blood samples (approximately 1.5 mL) were obtained in heparin and centrifuged to separate plasma from red blood cells. Plasma obtained was stored at 20°C before measurements were made.
Interleukin measurements
Plasma concentrations of IL-6, IL-8, and TNF-α were measured by enzyme-linked immunosorbent assay in 96-well microplates, using the Bender MedSystems (Vienna, Austria) kits BMS224, BMS213/2, BMS204, and BMS223/3. Standard curves were constructed and sample concentrations measured using the Plate Manager software from BioRad (Waltham, USA).
Statistical analysis
The data are expressed as mean and standard deviations. The results were analyzed to verify normality of distribution using the Kolmogorov–Smirnov test. The data were not normally distributed and all inferential analyses were made using non-parametric statistical tests. The Kruskal–Wallis test between the three groups was employed (FE, FT, SS) while Friedman’s test was employed to compare values at different time points in all three groups. For refusal of the null hypothesis, the Friedman and Kruskal–Wallis test was used. p values <0.05 were set as statistically significant. The CRIES score for the three groups were analyzed by using multivariate analysis of variance.
Results
From September 2007 to September 2009, 150 newborns of with gestational age 27 and 32 weeks, all white Caucasians were studied. The newborns did not differ significantly with respect to gestational age, birth weight or mean APGAR Index at 1 and 5 min. Also there were no differences with respect to sex, ante-natal steroid use or method of delivery.
Table 1 summarized the mean CRIES scores obtained with the three analgesic procedures. The reduction in the pain score was greater in the FE and SS group than that resulting from FS. The differences were statistically significant (p < 0.01).
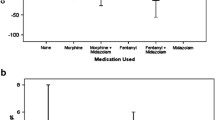
The secondary outcomes of the study were the levels of cytokines during the painful procedures including markers of stress correlated to pain. Figures 1, 2, and 3 summarize the changes in serum IL-6 and IL-8 and TNF-α, respectively, during the course of the study (0, 1, 3, and 7 days) in the three groups of newborns.
IL-6 concentrations at the onset of the study (0 time) were similar in all individuals of the three groups. IL-6 concentrations were significantly higher in the FT newborns at 1 day (p < 0.01), at 3 days (p < 0.01), and at 7 days compared with the FE and the SS-treated newborns. Also, in the newborns that received FE, the IL-6 concentrations were higher at all times compared to the SS group (p < 0.01; Fig. 1).
In reference to IL-8, this constituent was not detectable in any of the children at the onset of the study. However, IL-8 concentrations were significantly higher from 1 to 7 days (p < 0.01) in FT newborns than in the other two groups. At 1 day mean IL-8 values were 510 pg/mL in the FE group, 1,380 pg/mL in FT group and 160 pg/mL in the SS group; these values differ significantly (p < 0.01). The mean IL-8 values at 3 days were roughly 12-fold higher (1.220 vs 97 pg/mL) in the serum of the FT group when compared with the newborns with SS (Fig. 2).
The TNF-α values also differed between the groups at 1, 3 and 7 days of the treatment. At the onset of the study (0 time), TNF-α concentrations were similar in all individuals of three groups. At 1 day, mean TNF-α values were 9.9 pg/mL in FE group, 14.1 pg/mL in FT group, and 3.5 in the SS group; these values differ significantly (p < 0.01). The mean TNF-α values at 3 days were 14.9 pg/mL in FE group, 40.7 pg/mL in FT group, and 3.2 in the SS group; at 7 days the mean TNF-α values were roughly 40-fold higher (120 versus 3,1 pg/mL) in the serum of the facilitated tucking group when compared with the newborns with SS (Fig. 3).
Discussion
Neonatal intensive care involves a high number of diagnostic and therapeutic procedures which are associated with pain for the neonates concerned. It is important to prevent or treat pain in neonates whenever possible. Numerous pharmacological and non-pharmacological treatments may alleviate procedural pain in newborns [18, 58]. The approach to pain and stress in NICU has often been with infusion of an opiate with the knowledge of its potent analgesic effects and also with the hope that its sedative effect would be beneficial [41, 43, 46, 48].
Cardiovascular effects of fentanyl are minimal; significantly, it has very little effect on blood pressure, with a wide therapeutic index [10, 33, 41, 43, 48]. Fentanyl has not been studied as extensively as morphine, but it has been shown to limit pain scores and presumably provide comfort in ventilated neonates. It should be used with caution with attention toward potential complications in this population because of the rapid development of tolerance and chest wall rigidity. It may be more useful in hypotensive neonates [34].
The SS is a non-pharmacological treatment that has been well studied. SS addresses the neonate on a number of different sensory levels: tactile, auditory, olfactory, and orogustatory. The neonate is calmed during, and in particular after, a painful stimulus with a tactile stimulus that involves massaging his/her back and face. A few drops of a pleasant-smelling oil are spread onto the hands and used at the orogustatory level. During the massage, the child is also spoken to gently (auditory level). Furthermore, the infant is provided with a cotton wool stick which has been sprinkled with 10% glucose so that he/she can suck on it (olfactory level) [21]. In a study of 17 preterm neonates [11], the authors reported this intervention as being significantly more pain-relieving than when using distilled water and standard nursing. In particular, this intervention had a positive effect on crying, with the multisensorially stimulated preterms not expressing any crying reaction. However, Bellieni et al. [11] noted that SS and sucking plus oral glucose have the greater analgesic effect with respect to no intervention (p < 0.001). The effect of SS is statistically better than that of glucose plus sucking (p < 0.01). SS promotes interaction between nurse and infant and is a simple effective form of analgesia in the Neonatal Intensive Care Unit. Recently, Bellieni et al. [15] showed that, even without the use of perfume on the hands, SS was effective as an analgesic maneuver. It made no difference whether SS was performed by mothers who applied it for the first time or experienced nurses. SS is easy to learn and any caregiver (mother, paediatrician, or nurse) can effectively use it.
FT was tested in three studies with randomised samples of 30–40 preterm infants [22, 35, 60]. The authors describe FT as an effective pain-relieving intervention. FT leads to a significant reduction in the pulse rate. In one study, time to first quieting and total crying time were reduced significantly in comparison to the control group [22]. With regard to oxygen saturation, however, this intervention showed no effect [22, 35]. It is important to mention that Corff et al. [22] did not use an objective measurement tool, but based the assessment on heart rate, oxygen saturation and sleep/wake state. The other two studies used the Premature Infant Pain Profile as an outcome measure of pain. Among a group of 40 intubated and ventilated preterm neonates between 23 and 32 weeks gestation, FT during endotracheal suctioning achieved significant pain relief [60].
The primary outcome of this study was to measure pain using the CRIES score during heel-lances performed within 2 days of birth. The study outcome measures suggest that FE and SS provide superior analgesia in preterm neonates during procedural pain. For the two anaesthetic procedures, a 5-point difference in terms of CRIES median score compared with the FT (p < 0.001) was detected.
Secondary outcomes of this study include changes in serum IL-6, IL-8, and TNF-α during the course of the hospitalization (0, 1, 3, and 7 days). Several studies, however, have shown variable relationships between cytokines and clinical pain. Demonstration of correlations between CSF levels of IL-6 and postoperative pain [17], wound exudates levels of IL-6 and analgesic consumption after elective cesarean section [19], and IL-8 in seminal plasma and pain in chronic prostatitis/chronic pelvic pain syndrome [39] support a functional relationship. Cytokines are of importance in the integrated inflammatory cascade in the mediation of pain and hyperalgesia [59].
Tissue injury initiates the liberation of various inflammatory mediators and hyperalgesic substances including prostaglandins (PGs), cytokines, and chemokines [20, 23], which integrate the inflammatory response. Leukocyte migration to the injured area, which is a characteristic of the inflammatory response, is associated with pain and tenderness, and is involved in wound healing [29, 50, 61]. IL-6 plays a role in controlling leukocyte recruitment pattern during acute inflammation [36]. In vitro studies show that IL-6 secretion is induced by many other inflammatory mediators including IL-1β, TNF-α, and PGE2 [55]. In turn, IL-6 induces the release of chemokines and IL- 8 [47]. Inflammatory cytokines, including IL-6, are also involved in the modulation of pain [25]. In inflammatory pain models, IL-6 induces a short-lasting PG-dependent hyperalgesia [23] and local analgesia via opioid secretion, probably from inflammatory cells [24, 45, 51]. Most, if not all, nucleated cells are capable of synthesizing IL-6 at variable rates [25]. Chemokines, particularly IL-8, CCL2, and CXCL1, also participate in inflammatory hypernociception in experimental animals.
In our study IL-6, IL-8, and TNF-α were higher in the FT individuals group than in the FE or SS-treated infants at 1 day (p < 0.01), at 3 days (p < 0.01), and at 7 days (p < 0.01). When we compare the data only between FE and SS groups, the concentrations of IL- 6, IL-8, and TNF-α were significantly higher at 1 or 3 days of life in the FE group and they differed significantly (p < 0.001). The failure of PGs inhibition by FT and FE to interfere with the upregulation of any of these mediators may explain, in part, the analgesic effect observed with the use of SS in painful inflammatory conditions. Inhibition of one or more of the cytokines and chemokines as shown here to temporally correlate with pain onset may provide a novel strategy for analgesic pain therapy.
References
Adams HA, Hempelmann G (1991) The endocrine stress reaction in anesthesia and surgery-origin and significance. Anasthesiol Intensivmed Notfallmed Schmerzther 26:294–305
Anand KJ, Aynsley-Green A (1985) Metabolic and endocrine effects of surgical ligation of patentductus arteriosus in the human preterm neonate: are there implications for further improvement of postoperative outcome? Mod Probl Paediatr 23:143–147
Anand KJ, Hickey PR (1992) Halothane-morphine compared with high-dose sufentanil for anesthesia and postoperative analgesia in neonatal cardiac surgery. N Engl J Med 326:1–9
Anand KJ (1998) Clinical importance of pain and stress in preterm neonates. Biol Neonate 73:1–9
Anand KJS, McIntosh N, Lagercrantz H, Pelusa E, Young TE, Vasa R (1999) Analgesia and sedation in preterm neonates who require ventilatory support. Results from the NOPAIN trial. Arch Pediatr Adolesc Med 153:331–338
Anand KJ, Scalzo FM (2000) Can adverse neonatal experiences alter brain development and subsequent behaviour? Biol Neonate 77:69–82
Anand KJS, Hall RW, Desai N, Shephard B, Bergqvist L, Young TE, Boyle EM Carbajal R, Bhutani VK, Moore MB, Kronsberg SS, Barton BA, or the NEOPAIN Trial (2004) Effects of morphine analgesia in ventilated preterm neonates: primary outcomes from the NEOPAIN randomised trial. Lancet 363:1673–1682
Anand KJ, Aranda JV, Berde CB, Buckman S, Capparelli EV, Carlo W, Hummel P, Johnston CC, Lantos J, Tutag-Lehr V, Lynn AM, Maxwell LG, Oberlander TF, Raju TN, Soriano SG, Taddio A, Walco GA (2006) Summary proceedings from the neonatal pain-control group. Pediatrics 117:S9–S22
Aretz S, Licht C, Roth B (2004) Endogenous distress in ventilated full-term newborns with acute respiratory failure. Biol Neonate 85:243–248
Arnold JH, Truog RD, Scavone JM, Fenton T (1991) Changes in the pharmacodynamic response to fentanyl in neonates during continuous infusion. J Pediatr 119:639–643
Bellieni CV, Buonocore G, Nenci A, Franci N, Cordelli DM, Bagnoli F (2001) Sensorial saturation: an effective analgesic tool for heel-prick in preterm infants: a prospective randomized trial. Biol Neonate 80:15–18
Bellieni CV, Bagnoli F, Perrone S, Nenci A, Cordelli DM, Fusi M, Ceccarelli S, Buonocore G (2002) Effect of multisensory stimulation on analgesia in term neonates: a randomised controlled trial. Pediatr Res 51:460–463
Bellieni CV, Bagnoli F, Buonocore G (2003) Alone no more: pain in premature children. Ethics Med 19:5–9
Bellieni CV, Burroni A, Perrone S, Cordelli DM, Nenci A, Lunghi A, Buonocore G (2003) Intracranial pressure during procedural pain. Biol Neonate 84:202–205
Bellieni CV, Cordelli DM, Marchi S, Ceccarelli S, Perrone S, Maffei M, Buonocore G (2007) Sensorial saturation for neonatal analgesia. Clin J Pain 23:219–221
Bellù R, de Waal KA, Zanini R (2008) Opioids for neonates receiving mechanical ventilation. Cochrane Database of Systematic Reviews, Issue 1. Art. No: CD004212. doi:10.1002/14651858.CD004212.pub3
Buvanendran A, Kroin JS, Berger RA, Hallab NJ, Saha C, Negrescu C, Moric M, Caicedo MS, Tuman KJ (2006) Upregulation of prostaglandin E2 and interleukins in the central nervous system and peripheral tissue during and after surgery in humans. Anesthesiology 104:403–410
Carbajal R, Gall O, Annequin D (2004) Pain management in neonates. Expert Rev Neurother 4:491–505
Carvalho B, Clark DJ, Angst MS (2008) Local and systemic release of cytokines, nerve growth factor, prostaglandin E2, and substance P in incisional wounds and serum following cesarean delivery. J Pain 9:650–657
Chichorro JG, Lorenzetti BB, Zampronio AR (2004) Involvement of bradykinin, cytokines, sympathetic amines and prostaglandins in formalin-induced orofacial nociception in rats. Br J Pharmacol 141:1175–1184
Cignacco E, Hamers JP, Stoffel L, van Lingen RA, Gessler P, McDougall J, Nelle M (2007) The efficacy of non-pharmacological interventions in the management of procedural pain in preterm and term neonates. A systematic literature review. Eur J Pain 11:139–152
Corff K, Seideman R, Venkataraman S, Lutes L, Yates B (1995) Facilitated tucking: a nonpharmacologic comfort measure for pain in preterm neonates. J Obstet Gynecol Neonatal Nurs 24:143–147
Cunha FQ, Poole S, Lorenzetti BB, Ferreira SH (1992) The pivotal role of tumour necrosis factor alpha in the development of inflammatory hyperalgesia. Br J Pharmacol 107:660–664
Czlonkowski A, Stein C, Herz A (1993) Peripheral mechanisms of opioid antinociception in inflammation: involvement of cytokines. Eur J Pharmacol 242:229–235
De Jongh RF, Vissers KC, Meert TF, Booij LHDJ, De Deyne CS, Heylen RJ (2003) The role of interleukin-6 in nociception and pain. Anesth Analg 96:1096–1103
Dyke MP, Kohan R, Evans S (1995) Morphine increases synchronous ventilation in preterm infants. J Paediatr Child Health 31:176–179
Fitzgerald M, Millard C, MacIntosh N (1988) Hyperalgesia in premature infants. Lancet 1:292
Fitzgerald M, Millard C, McIntosh N (1989) Cutaneous hypersensitivity following peripheral tissue damage in newborn infants and its reversal with topical anaesthesia. Pain 39:31–36
Gillitzer R, Goebeler M (2001) Chemokines in cutaneous wound healing. J Leukoc Biol 69:513–521
Goldman RD, Koren G (2002) Biologic markers of pain in the vulnerable infant. Clin Perinatol 29:415–425
Goldstein RF, Brazy JE (1991) Narcotic sedation stabilizes arterial blood pressure fluctuations in sick premature infants. J Perinatol 11:365–371
Grunau R (2002) Early pain in preterm infants: a model of long-term effects. Clin Perinatol 29:373–394
Guinsburg R, Kopelman BI, Anand KJ, de Almeida MF, Peres Cde A, Miyoshi MH (1998) Physiological, hormonal, and behavioral responses to a single fentanyl dose in intubated and ventilated preterm neonates. J Pediatr 132:954–959
Hall RW, Boyle E, Young T (2007) Do ventilated neonates require pain management? Semin Perinatol 31:289–297
Huang CM, Tung WS, Kuo LL, Chang YJ (2004) Comparison of pain responses of premature infants to the heelstick between containment and swaddling. J Nurs Res 12:31–40
Hurst SM, Wilkinson TS, McLoughlin RM, Jones S, Horiuchi S, Yamamoto N, Rose-John S, Fuller GM, Topley N, Jones SA (2001) IL-6 and its soluble receptor orchestrate a temporal switch in the pattern of leukocyte recruitment seen during acute inflammation. Immunity 14:705–714
Jones JE, Kassity N (2001) Varieties of alternative experience: complementary care in the neonatal intensive care unit. Clin Obstet Gynecol 44:750–768
Kehlet H (1988) The modifying effect of anesthetic technique on the metabolic and endocrine responses to anesthesia and surgery. Acta Anaesthesiol Belg 39:143–146
Khadra A, Fletcher P, Luzzi G, Shattock R, Hay P (2006) Interleukin-8 levels in seminal plasma in chronic prostatitis/chronic pelvic pain syndrome and non-specific urethritis. BJU Int 97:1043–1046
Krechel SW, Bildner J (1995) CRIES: a new neonatal postoperative pain measurement score. Initial testing of validity and reliability. Paediatr Anaesth 5:53–61
Lago P, Benini F, Agosto C, Zacchello F (1998) Randomised controlled trial of low dose fentanyl infusion in preterm infants with hyaline membrane disease. Arch Dis Child Fetal Neonatal Ed 79:F194–F197
Menon G, Anand KJ, McIntosh N (1998) Practical approach to analgesia and sedation in the neonatal intensive care unit. Semin Perinatol 22:417–424
Orsini AJ, Leef KH, Costarino A, Dettore MD, Stefano JL (1996) Routine use of fentanyl infusions for pain and stress reduction in infants with respiratory distress syndrome. J Pediatr 129:140–145
Pokela ML (1994) Pain relief can reduce hypoxaemia in distressed neonates during routine treatment procedures. Pediatrics 93:379–383
Przewlocki R, Hassan AHS, Lason W, Epplen C, Herz A, Stein C (1992) Gene expression and localization of opioid peptides in immune cells of inflamed tissue: functional role in antinociception. Neuroscience 48:491–500
Quinn MW, Wild J, Dean HG, Hartley R, Rushforth JA, Puntis JW, Levene MI (1993) Randomised double-blind controlled trial of effect of morphine on catecholamine concentrations in ventilated pre-term babies. Lancet 342:324–327
Romano M, Sironi M, Toniatti C, Polentarutti N, Fruscella P, Ghezzi P, Faggioni R, Luini W, van Hinsbergh V, Sozzani S, Bussolino F, Poli V, Ciliberto G, Mantovani A (1997) Role of IL-6 and its soluble receptor in induction of chemokines and leukocyte recruitment. Immunity 6:315–325
Saarenmaa E, Huttunen P, Leppäluoto J, Meretoja O, Fellman V (1999) Advantages of fentanyl over morphine in analgesia for ventilated newborn infants after birth: a randomized trial. J Pediatr 134:144–150
Simons SH, van Dijk M, van Lingen RA, Roofthooft D, Duivenwoorden HJ, Johgeneel N, Bunkers C, Smink E, Anand KJ, van der Aker, Tibboel D (2003) Routine morphine infusion in preterm newborns who received ventilatory support: a randomized controlled trial. JAMA 290:2419–2427
Steed DL (1997) The role of growth factors in wound healing. Surg Clin North Am 77:575–586
Stein C, Hassan AHS, Przewlocki R, Gramsch C, Peter K, Herz A (1990) Opioids from immunocytes interact with receptors on sensory nerves to inhibit nociception in inflammation. Proc Natl Acad Sci USA 87:5935–5939
Stevens BJ, Johnston CC (1994) Physiological responses of premature infants to a painful stimulus. Nurs Res 43:226–231
Stevens B, Johnston C, Petryshen P, Taddio A (1996) Premature infant pain profile: development and initial validation. Clin J Pain 12:13–22
Stevens B, Gibbins S, Sturla Franck L (2000) Treatment of pain in the neonatal intensive care unit. Pediatr Clin North Am 47:633–650
Suganuma MM (2002) Discrete roles of cytokines, TNF-alpha, IL-1, IL-6 in tumor promotion and cell transformation. Int J Oncol 20:131–136
Tsuji M, Saul P, du Plessis A, Eichenwald E, Sobh J, Crocker R, Volpe JJ (2000) Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics 106:625–632
Uçeyler N, Sommer C (2008) Cytokine regulation in animal models of neuropathic pain and in human diseases. Neurosci Lett 437:194–198
Yamada J, Stinson J, Lamba J, Dickson A, McGrath PJ, Stevens B (2008) A review of systematic reviews on pain interventions in hospitalized infants. Pain Res Manag 13:413–420
Wang XM, Hamza M, Wu TX, Dionne RA (2009) Upregulation of IL-6, IL-8 and CCL2 gene expression after acute inflammation: correlation to clinical pain. Pain 142:275–283
Ward-Larson C, Horn R, Gosnell F (2004) The efficacy of facilitated tucking for relieving procedural pain of endotracheal suctioning in very low birthweight infants. Am J Matern Child Nurs 29:151–156
Watkins LR, Maier SF (2002) Beyond neurons: evidence that immune and glial cells contribute to pathological pain states. Physiol Rev 82:981–1011
Winberg J (1998) Do neonatal pain and stress program the brain’s response to future stimuli? Acta Paediatr 87:723–725
Conflict of interest statement
The authors declare that they have no conflict of interest. Authors have no a financial relationship with the organization that sponsored the research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gitto, E., Pellegrino, S., Manfrida, M. et al. Stress response and procedural pain in the preterm newborn: the role of pharmacological and non-pharmacological treatments. Eur J Pediatr 171, 927–933 (2012). https://doi.org/10.1007/s00431-011-1655-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-011-1655-7